Baldwin, Murphy Lead Call Urging Trump Administration to Cover COVID-19 Related Medical Expenses for Those Enrolled in Junk Plans
These Plans Have Left Patients with Potential and Confirmed COVID-19 Cases Saddled By High Medical Bills at a Time When the Economy and Many Livelihoods Are In Jeopardy
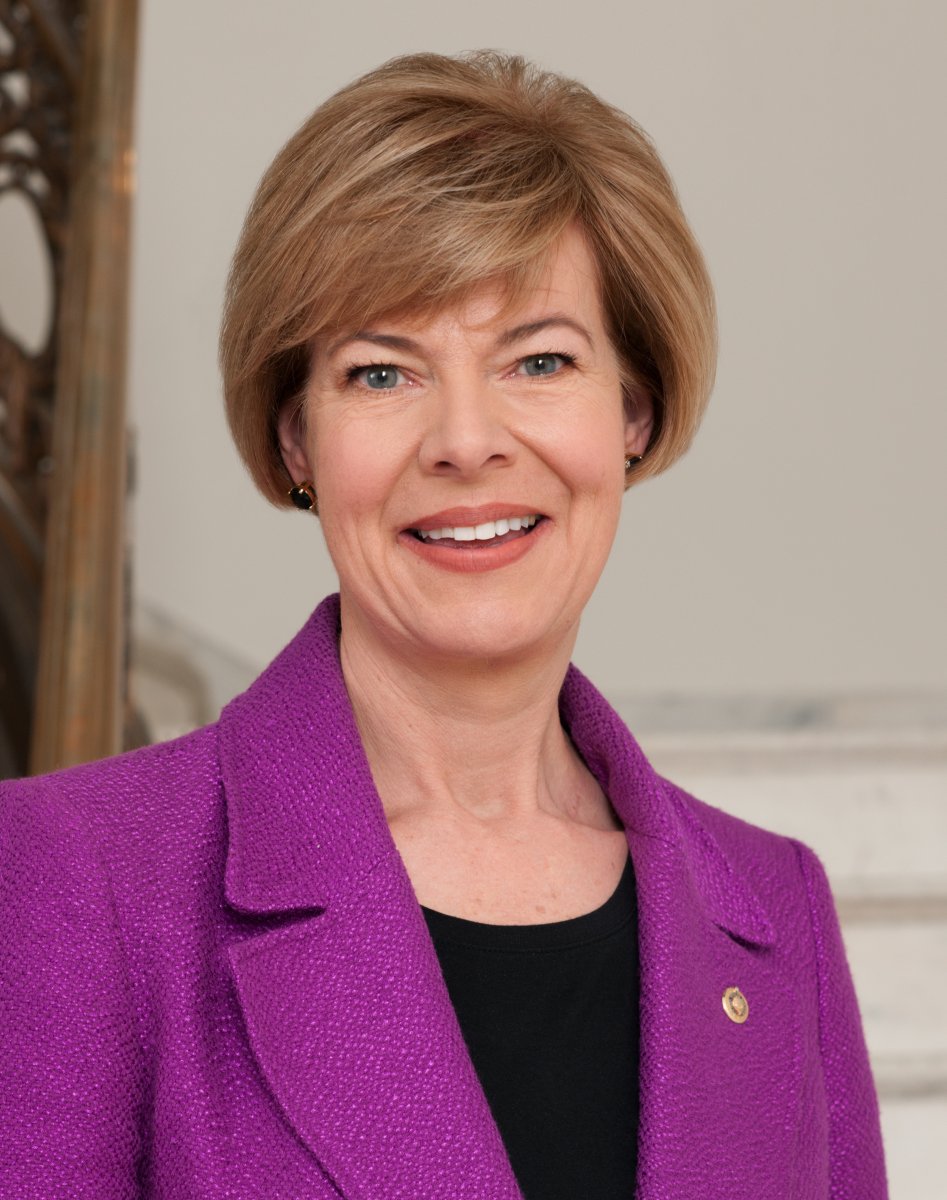
WASHINGTON, D.C. – U.S. Senators Tammy Baldwin (D-WI) and Chris Murphy (D-CT), both members of the Senate Health, Education, Labor and Pensions (HELP) Committee, on Friday led eight Senate Democrats in urging the Trump administration to cover the COVID-19 treatment expenses for those enrolled in short term, limited duration insurance (STLDI) plans. These so-called junk plans, which are heavily promoted by the administration, often do not cover essential medical services and are leaving consumers recovering from coronavirus with high out-of-pocket expenses. The administration has said it will exclude those enrolled in junk plans from theCARES Act uninsured relief fund even though it has the authority to cover these unanticipated, non-reimbursable expenses and it would be the right thing to do. Joining Baldwin and Murphy in sending this letter are Senators Mazie Hirono (D-HI), Tina Smith (D-MN), Elizabeth Warren (D-MA), Chris Van Hollen (D-MD), Tom Carper (D-DE), Sherrod Brown (D-OH), Jeff Merkley (D-OR), and Richard Blumenthal (D-CT).
“By excluding health care providers and facilities serving individuals enrolled in STLDI plans from COVID-19 claims reimbursement, you are adding to the financial liabilities of the underinsured. This decision, coupled with your decision to reject opening a special enrollment period, puts thousands of Americans at risk during a pandemic,”the senators wrote.
“The FFCRA defines uninsured as an individual who is not enrolled in Medicare, Medicaid, CHIP, TRICARE, VA health care, fully insured and self-insured individual and group health plans, and the Federal Employees Health Benefits Program. The definition in the statute excludes STLDI, treating them as uninsured for the purposes of COVID-19 testing coverage. This language makes clear that it is the intent of Congress to ensure that those enrolled in a STLDI plan are accounted for, and treated as uninsured to guarantee that they may access services critical for both individual patient care and the health of the public,” the senators added.
“Given the financial burden this decision will add to those enrolled in STLDI plans, we urge you to reconsider the decision not to cover their claims for COVID-19 testing and treatment. It is the least you should be doing to protect those individuals from unanticipated health care costs,” the members concluded.
The full letter is available here and below. An online version of this release is available here.
The Honorable Alex Azar
Secretary
U.S. Department of Health and Human Services
200 Independence Avenue SW
Washington, DC 20201
Dear Secretary Azar,
We write with grave concerns about your reported decision to deny those enrolled in short term, limited duration insurance (STLDI) plans, or junk plans, the federal resources appropriated for COVID-19 testing and treatment coverage. By excluding health care providers and facilities serving individuals enrolled in STLDI plans from COVID-19 claims reimbursement, you are adding to the financial liabilities of the underinsured. This decision, coupled with your decision to reject opening a special enrollment period, puts thousands of Americans at risk during a pandemic. We already have seen examples of how these plans, touted by your administration, have left patients with potential and confirmed COVID-19 cases saddled by high medical bills, at a time when the economy and many livelihoods are in jeopardy. We urge you to reconsider and expand coverage and protections to those enrolled in STLDI plans by including them for coverage as uninsured.
In the midst of a national health crisis, Americans need assurance that they will have comprehensive health insurance. STLDI plans do not provide this protection. This substandard health coverage promoted by the administration does not meet Federal consumer protection standards, including protections for pre-existing conditions, lifetime and annual dollar limits, and Essential Health Benefits (EHBs) like laboratory testing, emergency care, and hospitalization. This means these junk plans are allowed to discriminate against people with pre-existing conditions, women, and seniors, and often they do not cover benefits like mental health and addiction care or prescription drugs.
In response to a question about why the administration was not extending claims reimbursement for those enrolled in STLDI, an official from the Department of Health and Human Services (HHS) noted that many insurance companies have agreed to provide coverage for COVID-19 treatment at no cost-sharing. It is accurate that many insurance companies have extended coverage for their ACA-compliant plans, however, many companies have failed to provide the same extension for STLDI plans that they operate. Thus, these assurances from HHS of no cost-sharing do not apply to those enrolled in those plans. Individuals enrolled in these plans and at risk of COVID-19 are hit twice – first by their inadequate plan, which is not required to provide coverage for the type of COVID-19 testing and treatment they may need, and second, by this administration’s failure to provide a backstop for testing and treatment costs.
Given the financial burden this decision will add to those enrolled in STLDI plans, we urge you to reconsider the decision not to cover their claims for COVID-19 testing and treatment. It is the least you should be doing to protect those individuals from unanticipated health care costs.
Sincerely,
NOTE: This press release was submitted to Urban Milwaukee and was not written by an Urban Milwaukee writer. While it is believed to be reliable, Urban Milwaukee does not guarantee its accuracy or completeness.
More about the Coronavirus Pandemic
- Governors Tony Evers, JB Pritzker, Tim Walz, and Gretchen Whitmer Issue a Joint Statement Concerning Reports that Donald Trump Gave Russian Dictator Putin American COVID-19 Supplies - Gov. Tony Evers - Oct 11th, 2024
- MHD Release: Milwaukee Health Department Launches COVID-19 Wastewater Testing Dashboard - City of Milwaukee Health Department - Jan 23rd, 2024
- Milwaukee County Announces New Policies Related to COVID-19 Pandemic - County Executive David Crowley - May 9th, 2023
- DHS Details End of Emergency COVID-19 Response - Wisconsin Department of Health Services - Apr 26th, 2023
- Milwaukee Health Department Announces Upcoming Changes to COVID-19 Services - City of Milwaukee Health Department - Mar 17th, 2023
- Fitzgerald Applauds Passage of COVID-19 Origin Act - U.S. Rep. Scott Fitzgerald - Mar 10th, 2023
- DHS Expands Free COVID-19 Testing Program - Wisconsin Department of Health Services - Feb 10th, 2023
- MKE County: COVID-19 Hospitalizations Rising - Graham Kilmer - Jan 16th, 2023
- Not Enough Getting Bivalent Booster Shots, State Health Officials Warn - Gaby Vinick - Dec 26th, 2022
- Nearly All Wisconsinites Age 6 Months and Older Now Eligible for Updated COVID-19 Vaccine - Wisconsin Department of Health Services - Dec 15th, 2022
Read more about Coronavirus Pandemic here
Mentioned in This Press Release
Recent Press Releases by U.S. Sen. Tammy Baldwin
Baldwin Demands Vought, McMahon Stop Blocking $7 Billion for Afterschool Programs, K-12 Schools Across America
Jul 14th, 2025 by U.S. Sen. Tammy BaldwinTrump admin has withheld $80 million from Wisconsin from funding signed into law by President Trump in March
Report: Wisconsin Hospitals Will Lose $264 Million Annually Under Republicans’ Budget Bill
Jul 11th, 2025 by U.S. Sen. Tammy BaldwinBaldwin voted against bill that will kick over 270,000 Wisconsinites off their healthcare
Baldwin, Murkowski Introduce Bipartisan Bill to Protect Our Shoreline Communities
Jul 10th, 2025 by U.S. Sen. Tammy BaldwinBill reauthorizes program that provides essential data and resources for coastal communities to protect against storms, boost safety, and plan for the future