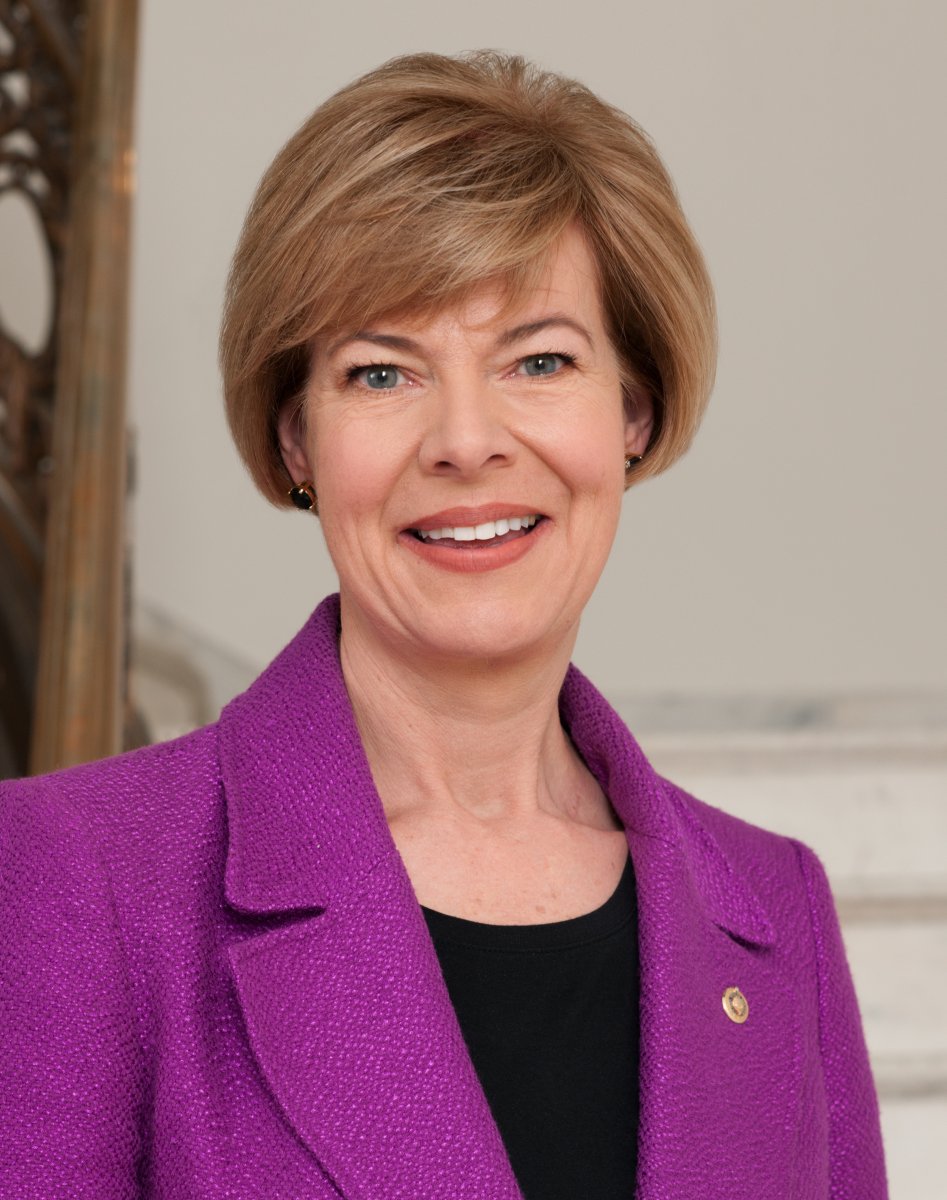
Baldwin Joins Effort to Review and Strengthen Medicare Advantage, Protect Taxpayers Dollars and Improve Care for Seniors
Recent federal audits show widespread overcharges and errors in payments across Medicare Advantage plans
WASHINGTON, D.C. – U.S. Senator Tammy Baldwin (D-WI) joined Senator Sherrod Brown (D-OH) and a group of Democratic colleagues in sending a letter to the U.S. Department of Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS), supporting CMS’s efforts to thoroughly examine current Medicare Advantage (MA) practices to improve care delivery for beneficiaries. Specifically, the letter urges the Administration to engage with stakeholders to strengthen and finalize proposals related to MA to reduce excessive payments to plans and bolster the Medicare program for all seniors and other beneficiaries.
“As you are aware, multiple federal audits and reports published over the last few years have identified a troubling trend of overpayments to MA plans, which are administered by private insurance companies. Federal audits made public in October 2022 revealed widespread overcharges and other errors in payments to these plans, totaling hundreds of millions of dollars in overcharges to the government in a manner that some have described as ‘cross[ing] the line into fraud,’” wrote the senators.
“We recognize that not all MA plans are engaged in unscrupulous or inappropriate care management, and that the number of Americans enrolled in MA plans continues to grow each year – approaching 50 percent of eligible beneficiaries. However, this shift in enrollment should not jeopardize the future of the Medicare program,” the senators continued.
For a copy of the letter, see below or here.
An online version of this release is available here.
Dear Secretary Becerra, Administrator Brooks-LaSure, and Deputy Administrator Seshamani:
We write in response to the Centers for Medicare & Medicaid Services’ (CMS) recent efforts to evaluate and improve the effectiveness and efficiencies in the Medicare program and strengthen the program to ensure it continues to meet the needs of the more than 65 million Americans who rely on Medicare for affordable, high-quality, person-centered care. We support CMS’s efforts to advance policies that will reduce waste and improve stewardship of Medicare funds and strengthen the benefit and quality of care for all enrollees, including the 34 million Americans who rely on traditional Medicare and the 30 million Americans who choose to enroll in a Medicare Advantage (MA) plan.
As you are aware, multiple federal audits and reports published over the last few years have identified a troubling trend of overpayments to MA plans, which are administered by private insurance companies. Federal audits made public in October 2022 revealed widespread overcharges and other errors in payments to these plans, totaling hundreds of millions of dollars in overcharges to the government in a manner that some have described as “cross[ing] the line into fraud.” A U.S. Department of Health and Human Services (HHS) Office of the Inspector General (OIG) report found that some insurance companies that offer MA plans are receiving billions in payments for health conditions captured on health risk assessments, but for which the plan does not provide any other care. And a recent report published by the Medicare Payment Advisory Commission (MedPAC) estimates that, absent any changes to current policy, taxpayers and Medicare beneficiaries will be on the hook for $27 billion in excessive and unwarranted payments to MA plans in 2023 alone, without any benefit to enrollees.
Beyond these reported overpayments that threaten the solvency of the Medicare program and jeopardize access for Medicare beneficiaries, we are also concerned by recent reports highlighting other troubling practices across some MA plans, impacting care delivery, timely payments to providers, and in some cases, putting seniors at risk. An April 2022 report from the HHS OIG estimated that over 85,000 medical prior authorizations that met Medicare coverage rules were improperly denied by a sample of MA plans in 2019.
We recognize that not all MA plans are engaged in unscrupulous or inappropriate care management, and that the number of Americans enrolled in MA plans continues to grow each year – approaching 50 percent of eligible beneficiaries. However, this shift in enrollment should not jeopardize the future of the Medicare program. We also appreciate that there are some nonprofit plans and smaller, regional MA plans that offer quality benefits to beneficiaries; in 2019, regional PPOs accounted for 6 percent of all MA enrollees. By focusing on mechanisms to protect the integrity of MA and improve the quality and timeliness of care for beneficiaries, CMS can ensure taxpayer dollars are protected and go toward strengthening benefits, increasing access to care, and lowering costs for beneficiaries as opposed to padding the profits of private companies.
As CMS works to strengthen and finalize proposals related to MA, we urge you to engage with stakeholders to ensure that any final policy changes ensure the program best serves the needs of enrollees and does not shift costs to other parts of Medicare or to taxpayers. We share your commitment to protecting and strengthening Medicare for all seniors and individuals with disabilities, and look forward to continuing to work with CMS to strengthen the Medicare benefit for current and future enrollees.
Sincerely,
NOTE: This press release was submitted to Urban Milwaukee and was not written by an Urban Milwaukee writer. While it is believed to be reliable, Urban Milwaukee does not guarantee its accuracy or completeness.
Mentioned in This Press Release
Recent Press Releases by U.S. Sen. Tammy Baldwin
On 3rd Anniversary of Roe Being Overturned, Baldwin, Blumenthal, and Murray Lead Senate Dems in a Bill to Restore Abortion Access Nationwide
Jun 24th, 2025 by U.S. Sen. Tammy BaldwinWomen’s Health Protection Act comes as Trump and Congressional Republicans move to restrict a woman’s right to choose and toward a national abortion ban
Baldwin Joins Bipartisan Group Urging Trump Admin to Reverse Closure of Job Corps Centers
Jun 23rd, 2025 by U.S. Sen. Tammy BaldwinBaldwin has been outspoken advocate for Wisconsin’s Job Corps centers that help young Americans get career training and are a path to good-paying jobs






















Recently on Thom Hartmann’s show I heard mention of an 85 year old WI woman named Francis Walter. Her Medicare Advantage plan use an algorithm to deny her coverage on her shattered left shoulder (she also had an allergy to pain medicine). The algorithm, not a doctor, estimated her recovery time to be 16.6 days, and then she would be ready to leave her nursing home.
“On the 17th day and following the algorithm, her Medicare Advantage insurer, Security Health Plan cut off payment for her care. From the algorithm results, Security was concluding she was ready to return to the apartment where she lived alone. Medical notes in June 2019 were showing Walter’s pain was maxing out the scales and that she could not dress herself, go to the bathroom, or even push a walker without help.
More than a year would pass before a federal judge decided the insurer’s decision was “at best, speculative.” And as such, Walter was owed thousands of dollars for the more than three weeks of treatment. She fought the insurer’s denial and while doing so, spent down her life savings to enroll in Medicaid and was able to progress to the point of putting on her shoes with her arm still in a sling”.
A Kaiser Family Foundation study found that gross margins among Medicare Advantage plans were more than double those of other markets, i.e., individual and group market plans as well as Medicaid managed plans. I like Tammy Baldwin but trying to make nice with corporate forces that are trying to ruin these “social safety net” programs in the name of profit isn’t going to work. George Dubya Bush’s Medicare Advantage needs to go. It’s not Medicare and it works to nobody’s advantage but the corporate profit motive behind it.