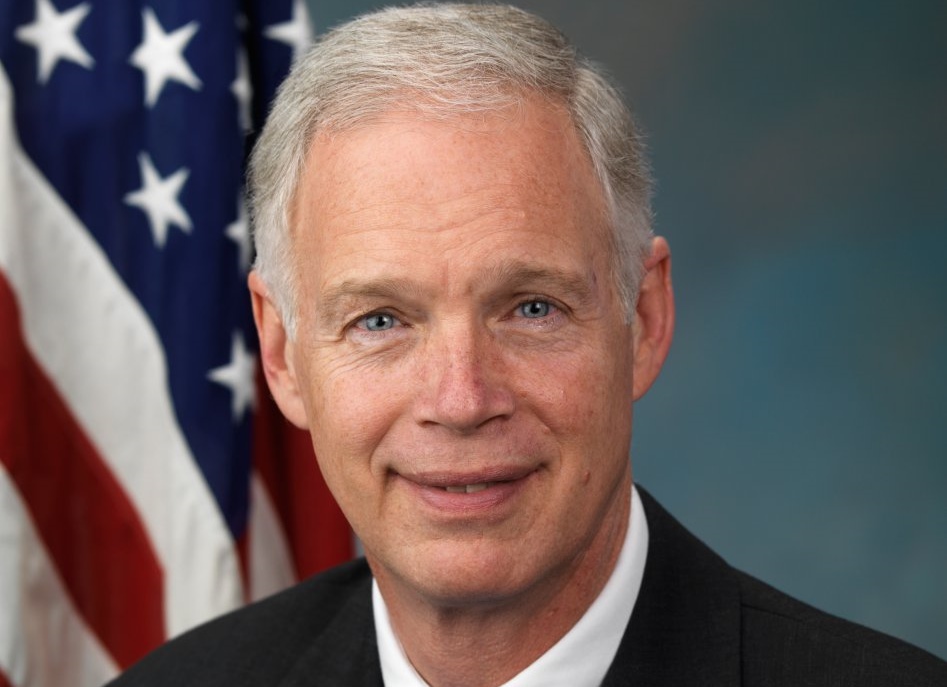
Johnson, Senators Send Letter to CMS Raising Alarm Over Growing Medicaid Improper Payments
WASHINGTON — U.S. Senators Ron Johnson (R-Wis.), chairman of the Senate Homeland Security and Governmental Affairs Committee, was joined by Sens. Lee (R-Utah), Paul (R-Ky.), Blackburn (R-Tenn.), Rick Scott (R-Fla.), Hyde-Smith (R-Miss.), Braun (R-Ind.), Lankford (R-Okla.), and Inhofe (R-Okla.) in sending a letter to Centers for Medicare and Medicaid Services (CMS) Administrator Seema Verma Tuesday to request a better understanding of how CMS is ensuring accountability in the Medicaid program after CMS reported its annual improper payment rates to Congress. The annual report estimated that $86.49 billion, or more than 21 percent of Medicaid payments were improper in fiscal year 2020 compared to $57.36 billion (14.9 percent) in Fiscal Year 2019 – a 50.8 percent increase.
A copy of the letter is available here and below.
December 22, 2020
The Honorable Seema Verma
Administrator
Centers for Medicare and Medicaid Services
200 Independence Avenue, S.W.
Washington, DC 20201
Dear Administrator Verma:
Over the last several years, we have highlighted areas where the Medicaid program is plagued by waste, abuse, and misspending.[1] On November 16, 2020, the Centers for Medicare and Medicaid Services (CMS) reported its annual improper payment rates to Congress.[2] This report validated our prior concerns regarding the rapid growth of Medicaid abuse and misspending following the passage and implementation of Obamacare.
In its report, CMS estimated that $86.49 billion, or more than 21 percent of Medicaid payments were improper in fiscal year 2020.[3] This compares to $57.36 billion (14.9 percent) in Fiscal Year 2019 – a 50.8 percent increase. As with prior years, the report confirmed that the dramatic increases of improper payments are mostly due to insufficient documentation to verify eligibility and income, or non-compliance with eligibility redetermination requirements.[4] This improper payment estimate includes eligibility audits for only two-thirds of states. According to recent reports, a complete accounting of the entire program would reveal an improper payment rate closer to 27 percent, or more than $100 billion in improper federal Medicaid spending.[5]
As the authors noted, Obamacare “created an incentive for states to view the Medicaid expansion population as a cash cow.”[9] Additionally, by canceling eligibility audits for four years, CMS removed the oversight necessary for states to administer Medicaid “responsibly or lawfully.”[10] The result of Medicaid expansion without proper accountability is staggering: Medicaid’s improper payment rates have more than tripled—from 6 percent to at least 21 percent—since the expansion of Medicaid under Obamacare in 2014.[11]
The magnitude of improper payments amplifies and reinforces the problems in the Medicaid program. Unfortunately, CMS has not taken steps to increase accountability, including withdrawing certain proposed corrective efforts and never completing others. This inaction has left Medicaid perpetually vulnerable to fraud and misuse and threatens the viability of the program for Americans truly in need.[12] To better understanding how CMS is ensuring accountability in the Medicaid program, please provide the following information and material:
- Please provide the improper payment rates, including the eligibility component of the rate, for all 50 states and the District of Columbia. This means the estimated improper payment rate by state for the one-third of states reviewed in 2017, the one-third of states reviewed in 2018, and the one-third of states reviewed in 2019.
- In areas where there is an above average level of improper Medicaid spending, please explain what actions that CMS has taken to date to ensure that only people who meet eligibility requirements are enrolled in the program. Separately, please describe what CMS plans to do in the future to ensure that only people who meet eligibility requirements are enrolled in the program.
- Please describe what steps, if any, that CMS has taken to recover the more than $143 billion of improper Medicaid payments identified by the 2019 and 2020 reports. Please provide the actions CMS has taken or plans to take to ensure corrective action in states where there is an above average level of Medicaid improper payments.
- On February 12, 2020, you wrote that some estimates of the fiscal impact from the Medicaid Fiscal Accountability Rule were alarmist and overblown.[13] However, in your announcement that the rule would be withdrawn, you noted concerns raised by state and provider partners about potential unintended consequences of the proposed rule that required further study.[14] Please explain the potential unintended consequences and the factors that changed CMS’ position on the rule.
Please provide this material as soon as possible but no later than 5:00 p.m. on January 6, 2020. Thank you for your attention to this matter.
###
[1] See, e.g., Letter from Sen. Ron Johnson, Chairman, S. Comm. on Homeland Sec. & Governmental Affairs, to Hon. Seema Verma, Admin’r, Ctr. For Medicare and Medicaid Serv. (Jun. 26, 2019), https://www.hsgac.senate.gov/imo/media/doc/2019-06-25%20RHJ%20to%20CMS%20re%20Medicaid%20Program%20Integrity%20One-Year%20Anniversary.pdf.
[2] Center for Medicare and Medicaid Services, Newsroom, 2020 Estimated Improper Payment Rates for Center for Medicare and Medicaid Services (CMS) Programs (Nov. 16, 2020), https://www.cms.gov/newsroom/fact-sheets/2020-estimated-improper-payment-rates-centers-medicare-medicaid-services-cms-programs.
[3] Id.
[4] Id.
[5] Brian Blasé, Medicaid is Hemorrhaging $100B on Americans Ineligible for the Program, NY Post (Nov. 28, 2020, 1:01 PM), https://nypost.com/2020/11/28/medicaid-hemorrhaging-100b-on-americans-ineligible-for-the-program/.
[6] Brian Blase and Aaron Yelowitz, Why Obama Stopped Auditing Medicaid, Wall Street Journal (Nov. 18, 2020, 7:05 PM), https://www.wsj.com/articles/why-obama-stopped-auditing-medicaid-11574121931.
[7] Id.
[8] Id.
[9] Id.
[10] Id., see also, e.g., RHJ 2019 letter.
[11] Id.
[12] Administrator Seema Verma (@SeemaCMS), Twitter (Sep. 14, 2020, 3:45 PM), https://twitter.com/SeemaCMS/status/1305608634165010443.
[13] Center for Medicare and Medicaid Services, Blog, 2020 Medicaid Fiscal Integrity: Protecting Taxpayers and Patients (Feb. 12, 2020), https://www.cms.gov/blog/medicaid-fiscal-integrity-protecting-taxpayers-and-patients.
[14] Supra note 11.
NOTE: This press release was submitted to Urban Milwaukee and was not written by an Urban Milwaukee writer. While it is believed to be reliable, Urban Milwaukee does not guarantee its accuracy or completeness.