State’s Failures On Lead Pipes
Legislature misses chance to take action, state cuts funding that helps protect kids.

Tory Lowe helped to organize a meeting about lead in drinking water at the House of Prayer in Milwaukee on Dec. 6. He asked the young boys in the audience to join him at the front of the room to challenge everyone to protect them from the dangers of lead in drinking water. The children, from left, are Tomairus Brown, 5, Diamante Silas, 7, Jakoda Eiland, 8, and Jeriko Eiland, 11. Photo by Coburn Dukehart of the Wisconsin Center for Investigative Journalism.
Fearing that lead from drinking water had poisoned their children, nearly 30 people gathered on a December evening to press for answers.
The event at the House of Prayer, a small church on Milwaukee’s northwest side, was organized by Tory Lowe, a community activist working to raise awareness of lead-in-water issues.
Evanny Dorsey, one of the mothers who spoke, said her daughter Avanny tested as having lead poisoning three times in the past year. Dorsey’s north side home is among the more than 70,000 homes, businesses and day care centers in Milwaukee with lead service lines.
“My baby is not the average 2-year-old, and I’ve kind of seen her behavior changing,” Dorsey said, adding that Avanny, who has since turned 3, has trouble paying attention and is talking less than other children her age.
Residents like Dorsey believe officials are not doing enough to prevent lead poisoning, which afflicts thousands of Wisconsin’s children each year.
The Wisconsin Center for Investigative Journalism has found state officials have declined to take actions that could better protect children like Avanny from lead in drinking water. Documents and interviews show that:
- Funding for the state’s Childhood Lead Poisoning Prevention Program has shrunk to “below optimal staffing,” according to a state Department of Health Services budget request that unsuccessfully sought additional funding in 2015-17. While Gov. Scott Walker’s administration has increased state funding to partially make up for sharp drops in federal grants, the program remains 23 percent smaller than it was in 2011, and there are no plans to ask for more money in the upcoming 2017-19 state budget.
- A recent public health campaign by DHS on lead poisoning prevention did not mention drinking water as a potential source of lead, despite the dangers illustrated by the Flint, Michigan lead-in-water crisis.
- State law does not mandate that drinking water be investigated as the source when a child is found to have lead poisoning. A bill that would have lowered the level of lead poisoning that triggers an investigation and require that water, in addition to paint, be examined as a source died in the Legislature in 2016 without a hearing. Currently, an investigation is triggered only after a child’s blood lead level reaches at least three times the amount that indicates lead poisoning — and even then, water is not required to be tested.
- The DHS is using an outdated, lax standard to determine which lead-poisoned children need medical and public health services.
- A proposal to study lead-poisoned infants in Milwaukee to determine whether drinking water was the cause was scrapped by the DHS in 2016. The agency said it decided against the study because it would not have differentiated the effects of lead paint from lead plumbing, both of which can be found in old homes.
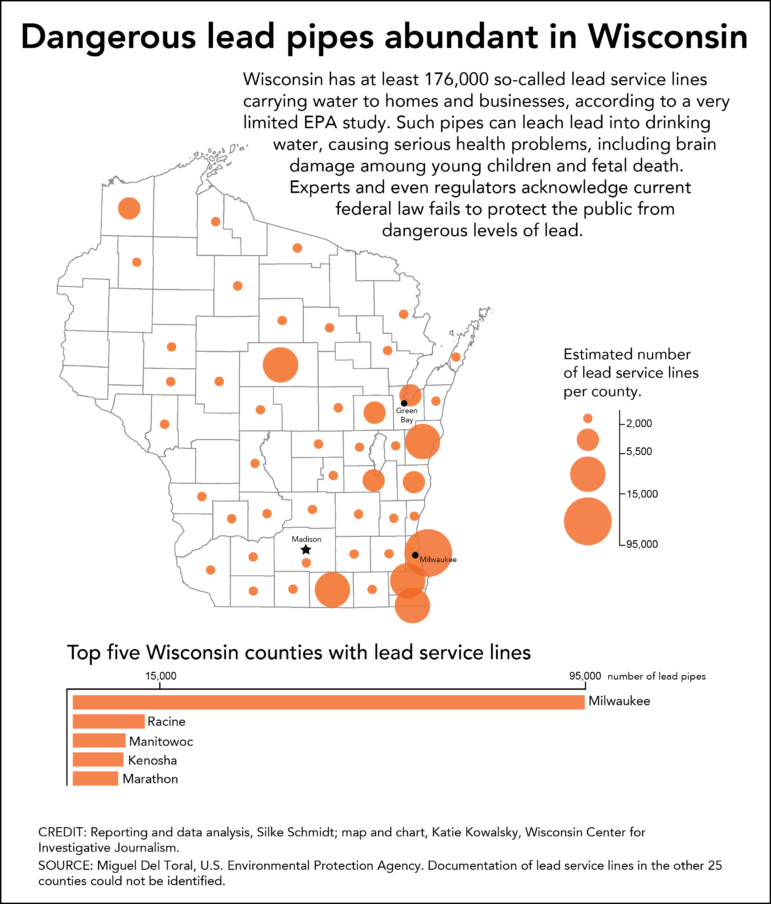
The risk of lead in drinking water goes beyond Milwaukee and spans dozens of communities across Wisconsin. Statewide, 4.5 percent of children tested were found to be lead poisoned in 2014, compared to the 4.9 percent of Flint children tested in 2015. Blood lead levels of 5 micrograms per deciliter of lead means the child has been lead poisoned.
In Milwaukee, 8.6 percent of children tested had blood lead levels at or above the level that indicates lead poisoning in 2014 — significantly higher than in Flint.
DHS spokeswoman Julie Lund rejected the idea that the agency was not doing enough to protect children from lead in drinking water. Lund said DHS has “taken a proactive stance” by working with state agencies, local health departments and the public, offering technical assistance and help with public health messaging.
“While we have made much progress in the detection and prevention of childhood lead poisoning, DHS staff is committed to working aggressively on this issue until the risk of lead poisoning is eliminated for all children,” she said. “For this reason, the DPH (Division of Public Health) is continuing to review all options available and what additional work can be done with existing resources.”
In reaction to the Center’s findings, three experts said the lack of attention in Wisconsin to protecting children from lead in drinking water is common across the nation.
Dr. Susan Buchanan, director of the Great Lakes Center for Children’s Environmental Health at the University of Illinois-Chicago, said agency budgets have been hit hard by the U.S. Centers for Disease Control and Prevention’s decision in recent years to slash funding for lead prevention efforts. One reason: Lead poisoning among children has dropped significantly since lead was removed from paint in 1978 and phased out and eventually removed from gasoline in 1995.
“Up until Flint happened,” Buchanan said, “I didn’t think much about water (as a contributor to lead poisoning) either.”
Scientist and activist Yanna Lambrinidou said public health officials nationwide have long ignored or underplayed the problem of lead in drinking water.
“My experience, sadly, is that when it comes to lead in water, the public health community is by and large keeping its head in the sand, deeply and doggedly,” said Lambrinidou, an affiliate Virginia Tech University faculty member. “Public health experts systematically downplay the risks of lead in water and succeed in convincing lawmakers, government officials and the public alike that this hazard deserves minimal, if any, attention.”
Lambrinidou’s Virginia Tech colleague, Marc Edwards, agreed.
“Public health agencies have continued to assert that the government-owned lead pipes, which contaminate potable water, pose an insignificant health risk,” said Edwards, an engineering professor who worked with Lambrinidou on the Flint water crisis. “Most of their energy has been directed to making sure that public funding and attention stays focused on lead paint mitigation, which is already a multi-billion-dollar-a-year industry that they are both familiar and comfortable with.”
Lead dangerous, damage permanent
The effects of lead poisoning, which are permanent, can include reduced mental development, behavioral problems and stunted growth. Children can become lead poisoned by ingesting paint, or lead-tainted water, soil or dust, but prevention and mitigation efforts have historically focused on paint.
Dorsey said she now buys bottled water for drinking but continues to cook meals with tap water because of the cost. Boiling water with lead in it is not recommended as it can actually concentrate the level of the neurotoxin.

Evanny Dorsey spoke at a meeting about lead in drinking water at the House of Prayer in Milwaukee on Dec. 6. She says her daughter, Avanny, age 3, has tested positive for elevated levels of lead three times in the past year. Because Avanny’s blood lead levels were just below the limit that would trigger an inspection, no one has been to Dorsey’s house to look for the source of lead. Dorsey suspects it’s leaching into the water from her home’s lead service lines. “It’s our future,” she said. “It’s our children that it’s affecting.” Photo by Coburn Dukehart of the Wisconsin Center for Investigative Journalism.
After tests showed Avanny was lead poisoned, health workers advised Dorsey to keep her daughter away from windowsills that might contain lead paint, feed her more vegetables and run tap water for 30 seconds before using it. No one has visited her home to inspect it or test her water, she said.
Dorsey believes she knows the source: lead from service lines that deliver water both to her home and the day care center that Avanny attends.
“You all spend the money on streetcars, and stadiums need to be built, but you all need to be putting this money that you all taking from us taxpayers and put it in our homes,” Dorsey said at the Milwaukee gathering in December as she fought back tears. “I know it’s a small room of us. There’s supposed to be way more of us. Because it’s way more communities that are affected, not only poor homes. It’s the whole community.”
Health agency downplays lead in water
Wisconsin’s childhood lead prevention program has shrunk since the federal government began sharply reducing funding in 2012. Although the Walker administration has added state money to the program, the overall size of the prevention effort, $1.6 million annually, is now 23 percent smaller than in 2011.
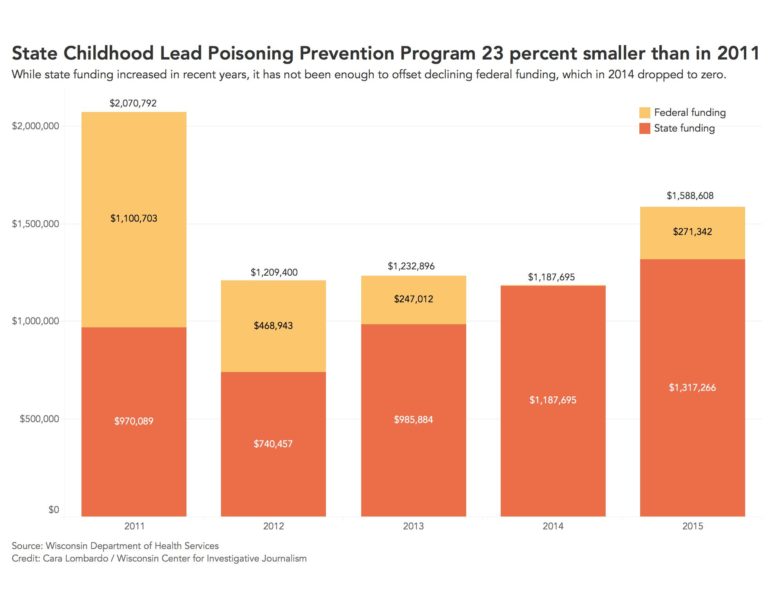
State Childhood Lead Poisoning Prevention Program 23 percent smaller than in 2011
State Childhood Lead Poisoning Prevention Program 23 percent smaller than in 2011.
Lund defended the current funding level, saying, “As federal funding was cut, the state has invested more.” She said the agency has no plans to ask for additional money for lead poisoning prevention in the upcoming 2017-19 budget.
The Economic Policy Institute has estimated that each $1 spent on lead hazard control results in net benefits of between $17 and $221 in increased lifetime earnings, higher tax revenue and lower costs for health care, special education and crime. The nonprofit think tank based in Washington, D.C. focuses on the needs of low- and middle-income workers in economic policy discussions.
In October, DHS issued a brochure for Childhood Lead Poisoning Prevention Week that did not mention drinking water as a potential source. Spokeswoman Jennifer Miller said lead paint is the “primary cause of lead poisoning among children in Wisconsin” and is the agency’s focus for prevention efforts.
“We are unaware of any cases of lead in drinking water as the primary cause of lead poisoning,” Miller said.
Lund said, however, that the agency continues to review new studies about the risk of lead in drinking water and is “re-evaluating public health messaging on this important topic.”

In February, State Rep. LaTonya Johnson introduced a bill that would require the state to conduct tap water testing when a child is lead poisoned and would lower the level of lead in a child’s blood at which the state would be required to investigate its source. The bill was never brought up for a vote. Johnson, who used to run a day care center in her Milwaukee home, says she provided water from a cooler to the children in her care to avoid exposure to lead. Johnson now serves in the state Senate. Photo by Coburn Dukehart of the Wisconsin Center for Investigative Journalism.
One reason the state finds no documented cases: Wisconsin does not require that drinking water be tested during investigations triggered when a child has severe lead poisoning. Lund said DHS is “considering” whether to require that drinking water be included when a local health department conducts an investigation for a lead-poisoned child.
In 2016, the state Department of Health Services also scrapped a proposed study that would have explored the links between Milwaukee infants who had been lead poisoned over the past 20 years and whether they had lived in homes with lead service lines, according to records obtained by the Center under the public records law. The theory is that infants aged 7 months and younger are not independently mobile and would not have easy access to lead paint, dust or soil.
Milwaukee Health Department spokeswoman Sarah DeRoo said the proposal was “exploratory,” and the state never identified a funding source. Lund said the agency dropped the idea because it was “unable to see any discernible patterns in the data that would have significantly helped to prevent or eliminate lead exposure in children.”
Legislative efforts stall
Last February, state Rep. LaTonya Johnson of Milwaukee, who is now a state senator, and other Democratic lawmakers introduced a bill that would have required the state to conduct tap water testing when a child is lead poisoned.
Johnson’s measure also would have lowered the level of lead in a child’s blood that would have required that water be investigated when a child is lead poisoned. The requirement, which would have cost state and local health departments about $4.8 million a year, was never brought up for a vote.
In Wisconsin, investigations are only required if the child’s blood lead level exceeded 15 micrograms per deciliter twice over 90 days or 20 micrograms once —and again, water is not required to be tested. The CDC recommended in 2012 that states lower that level to 5 micrograms.
In an August response, the agency said it was “reviewing its options.” By December, Lund told the Center that the agency would be updating the threshold. But she emphasized DHS is not authorized to change the requirements for a lead investigation; that is up to the Legislature.
Had lawmakers acted, Avanny Dorsey’s blood lead levels just under 10 micrograms per deciliter would have triggered an investigation into how she got lead poisoned, including whether it came from drinking water.
Evanny Dorsey, who is expecting another child, worries about the dangers using water from lead pipes. She said officials should remove them as soon as possible.
“If it takes breaking down the whole community and rebuilding houses just to get those lead pipes out, that’s what it’s going to take to get the lead out of our children,” Dorsey said, adding, “It’s our future. It’s our children that it’s affecting.”
The nonprofit Wisconsin Center for Investigative Journalism (www.WisconsinWatch.org) collaborates with Wisconsin Public Radio, Wisconsin Public Television, other news media and the UW-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by the Center do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.
More about the Lead Crisis
- Rep. Madison Proposes Restoring Local Control Over Lead Inspections - State Rep. Darrin Madison - Jan 6th, 2026
- $43 Million Later, MPS Says Classrooms Are Safe From Lead Dust - Corrinne Hess - Dec 18th, 2025
- MPS Buildings Cleared of Lead-Paint Risks after 10-Plus Months of Work - Milwaukee Public Schools - Dec 17th, 2025
- Wisconsin Moves to Require Lead Service Lines Replaced By 2037 - Danielle Kaeding - Dec 11th, 2025
- Gov. Evers, DNR Announce More Than $159 Million to Ensure Clean, Safe Drinking Water for Wisconsinites in 29 Municipalities - Gov. Tony Evers - Dec 10th, 2025
- EPA Announces $3 Billion in New Funding for States to Reduce Lead in Drinking Water - U.S. Environmental Protection Agency - Nov 25th, 2025
- Wisconsin Communities Get $282 Million for Drinking Water Projects - Danielle Kaeding - Nov 19th, 2025
- MKE County: County Launches Lead Abatement Program - Graham Kilmer - Nov 9th, 2025
- Milwaukee County Launches Lead Remediation Program to Reduce Lead-Based Paint Hazards in Homes in Suburban Communities - David Crowley - Nov 5th, 2025
- Wisconsin Improves Child Lead Testing Rates, Urges Continued Testing and At-Home Prevention - Wisconsin Department of Health Services - Oct 21st, 2025
Read more about Lead Crisis here
Tainted Water
-
Fecal Microbes In 60% of Sampled Wells
 Jun 12th, 2017 by Coburn Dukehart
Jun 12th, 2017 by Coburn Dukehart
-
Lax Rules Expose Kids To Lead-Tainted Water
 Dec 19th, 2016 by Cara Lombardo and Dee J. Hall
Dec 19th, 2016 by Cara Lombardo and Dee J. Hall
-
DNR Program Replaces Lead Laterals
 Dec 19th, 2016 by Cara Lombardo and Dee J. Hall
Dec 19th, 2016 by Cara Lombardo and Dee J. Hall



















There is another culprit in the story of lead in our water: the lead industry. For decades after the lead companies – including NL Industries, ASARCO and Eagle Picher – knew that lead pipes could cause lead poisoning they continued to sell and promote lead pipes. (see The Lead Industry and Lead Water Pipes: “A Modest Campaign”; Am J Public Health. 2008;98:1584–1592) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2509614/