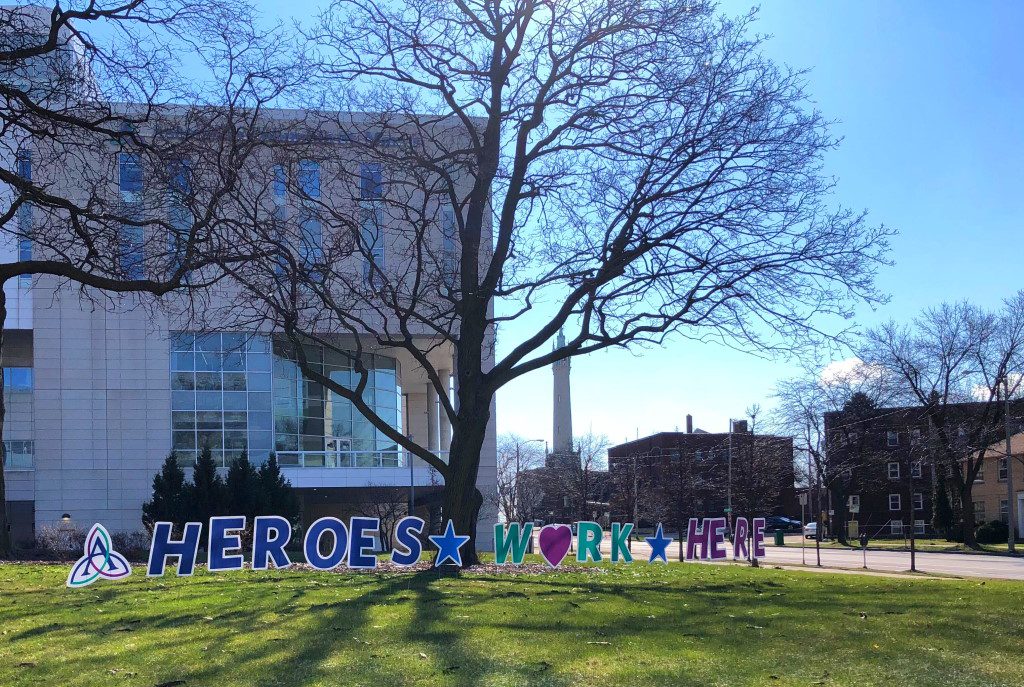
Hospitals, Nursing Homes Facing Staff Shortages
When healthcare workers contract COVID-19 it exacerbates existing staff shortages.
Faced with staff shortages in hospitals, nursing homes and other long-term care facilities during the COVID-19 pandemic, state health officials and hospital administrators are hunting for ways to recruit more workers.
Hospitals are holding patients who are ready to be discharged but have nowhere to go, because they need to go to long-term care — and nursing homes or other long-term care facilities aren’t able to take them.
That’s not strictly a new problem.
“There’s always been a staffing shortage” in nursing homes, says Rick Abrams, president of the Wisconsin Health Care Association / Wisconsin Center for Assisted Living (WHCA/WiCAL), a long-term care trade group. “Even before the pandemic hit, the average vacancy rate was 23%. COVID has exacerbated what was already an acute shortage.”
“What we have heard consistently from our hospitals is the biggest issue is staff,” said Julie Willems Van Dijk, deputy secretary of the Wisconsin Department of Health Services (DHS) at a department media briefing Thursday. “They have beds, they don’t have staff — and that is true in long-term care.”
Chronic staffing challenges have been exacerbated by the pandemic as healthcare workers, in nursing homes as well as hospitals and clinics, have either contracted COVID-19 in the community or been exposed to others who have tested positive for the coronavirus.
People who have been exposed must quarantine for up to two weeks to guard against spreading the virus, and people who have tested positive must isolate until they are clear of the virus.
The pandemic’s surge showed no signs of letting up Thursday.
At the DHS media briefing, Gov. Tony Evers recapped his Tuesday night address to the state, again urging state residents to stay home, stay physically distant from people outside their household, wear masks in public and wash hands frequently.
“If we don’t treat this pandemic like the urgent crisis it is, Wisconsin could lose thousands more of our friends, family loved ones and fellow Wisconsinites by the end of the year,” the governor said.
Evers declined to discuss details of legislation his office has been developing to provide additional relief during the pandemic, but said he expected it to be read by the beginning to middle of next week. He also said he intended to share it with leaders of the Assembly and the Senate, “so that we can actually accomplish some things.”
As of Thursday, DHS reported 7,497 new cases of COVID-19 and 58 new deaths. The number of people confirmed positive for COVID-19 now stands at 293,388 and appears likely to top 300,000 this weekend if not sooner. The total number of deaths now stand at 2,515
Wisconsin hospitals had 2,077 patients with COVID-19 Thursday, according to the Wisconsin Hospital Association (WHA). Of those, 424 patients were in intensive care. The numbers reflected a minuscule improvement, however: a decrease of 25 patients overall from Wednesday, with 17 fewer ICU patients.
But the pressure remains on hospitals, even as more patients might be able to leave if they had somewhere else to go.
Around the state, “patients who are medically ready for discharge and transfer from the inpatient setting to long-term care facility settings are being held in the hospital, because long-term care facility beds, nursing home beds, are not available,” said Dr. Mark Kaufman, chief medical officer for the WHA, in an interview with the Wisconsin Examiner earlier this week.
“That impacts both COVID patients and non-COVID patients in the hospital,” Kaufman said. “If you have reduced bed capacity in the hospital, those beds aren’t available for both COVID patients and non-COVID patients.”
“The system is bordering on freezing up and we can’t allow that to happen,” says Abrams, the WHCA/WiCAL president.
An Alternate Care Facility at State Fair Park in West Allis, which the state set up for recovering COVID-19 patients who were well enough to leave an acute-care hospital but not quite ready to go home, had 14 patients as of Thursday, with room for more than 500 eventually.
Willems Van Dijk said Thursday that the state is considering changes in the admission criteria to make further use of the West Allis facility, although not as a substitute for long-term care.
Kaufman and Abrams agreed that there would be little reason to open such a facility for patients ready for long-term care, but for whom a nursing home bed could not be found — because the problem is staffing, not space.
Willems Van Dijk said DHS and healthcare providers, including nursing homes, are working on a number of strategies to ease the staffing shortage.
The agency and providers have asked the Federal Emergency Management Agency (FEMA) to help with placing additional healthcare workers.
“We’re working on a number of initiatives to bring further nursing assistants into the state workforce, reaching out to people who have lapsed certificates or licenses, finding ways to better hire people from across state lines,” the DHS deputy secretary said.
And, she added, the state is examining “how we can safely bring people who are in quarantine back to healthcare work with appropriate testing and PPE” — personal protective equipment.
The new funds “will be able to ensure that the facilities will be able to retain the staff they’ve got,” Abrams says, including overtime for existing staff and temporary help if needed.
When it comes to the surge, however, state officials are emphasizing that while they hunt for more healthcare workers or consider what new needs there are for space, preventing more illness remains the top priority.
“We need to go back to how we stopped the patients from coming to the hospital in the first place,” Willems Van Dijk said. “And so let’s not forget that it’s on each of us to take action to plateau and decrease the spread of the disease, which will decrease the source of this surge in the first place.”
Reprinted with permission of Wisconsin Examiner.
More about the Coronavirus Pandemic
- Governors Tony Evers, JB Pritzker, Tim Walz, and Gretchen Whitmer Issue a Joint Statement Concerning Reports that Donald Trump Gave Russian Dictator Putin American COVID-19 Supplies - Gov. Tony Evers - Oct 11th, 2024
- MHD Release: Milwaukee Health Department Launches COVID-19 Wastewater Testing Dashboard - City of Milwaukee Health Department - Jan 23rd, 2024
- Milwaukee County Announces New Policies Related to COVID-19 Pandemic - David Crowley - May 9th, 2023
- DHS Details End of Emergency COVID-19 Response - Wisconsin Department of Health Services - Apr 26th, 2023
- Milwaukee Health Department Announces Upcoming Changes to COVID-19 Services - City of Milwaukee Health Department - Mar 17th, 2023
- Fitzgerald Applauds Passage of COVID-19 Origin Act - U.S. Rep. Scott Fitzgerald - Mar 10th, 2023
- DHS Expands Free COVID-19 Testing Program - Wisconsin Department of Health Services - Feb 10th, 2023
- MKE County: COVID-19 Hospitalizations Rising - Graham Kilmer - Jan 16th, 2023
- Not Enough Getting Bivalent Booster Shots, State Health Officials Warn - Gaby Vinick - Dec 26th, 2022
- Nearly All Wisconsinites Age 6 Months and Older Now Eligible for Updated COVID-19 Vaccine - Wisconsin Department of Health Services - Dec 15th, 2022
Read more about Coronavirus Pandemic here




















Perhaps higher wages would bring more interest from prospective employees.