Pressure Builds on State’s Hospitals
More than 95% of ICU beds are full, one-third of them patients with COVID-19.
As COVID-19 cases continue to spread, the state health department raised the alarm Monday that even more rapid spread is likely soon. Dane County, the only county in Wisconsin with a mask requirement, extended it for another month. Meanwhile, Wisconsin’s highest court set the stage for a new challenge to local public health orders.
The actions all came as health officials warned of a continued COVID-19 pandemic surge, swamping hospitals and raising the risk that people needing medical care — not just for COVID-19, but for other life-threatening conditions — would be turned away.
The agency stated: “There is a serious risk that continued, increased numbers of COVID-19 cases will overwhelm an already strained health care system, leading to dangerous situations where patients experiencing medical emergencies may not be able to receive immediate, adequate, lifesaving attention and care due to the lack of hospital capacity.”
As of Sunday, Wisconsin has recorded an average of 3,294 new cases each day for the last seven days. “This is nearly double where we were only two months ago,” said Karen Timberlake, DHS secretary-designee, at a department briefing on the pandemic Monday afternoon.
“We are seeing daily case numbers that we haven’t seen since the end of last year,” Timberlake said. “High rates of COVID-19 transmission are occurring in all Wisconsin counties. And that trajectory is growing.”
The total number of confirmed cases in Wisconsin since the pandemic began reached 943,355 as of Sunday, DHS reported. The seven-day average for COVID-19 deaths per day in Wisconsin was 28 as of Sunday, and it is the confirmed cause of death for 9,683 people in the state.
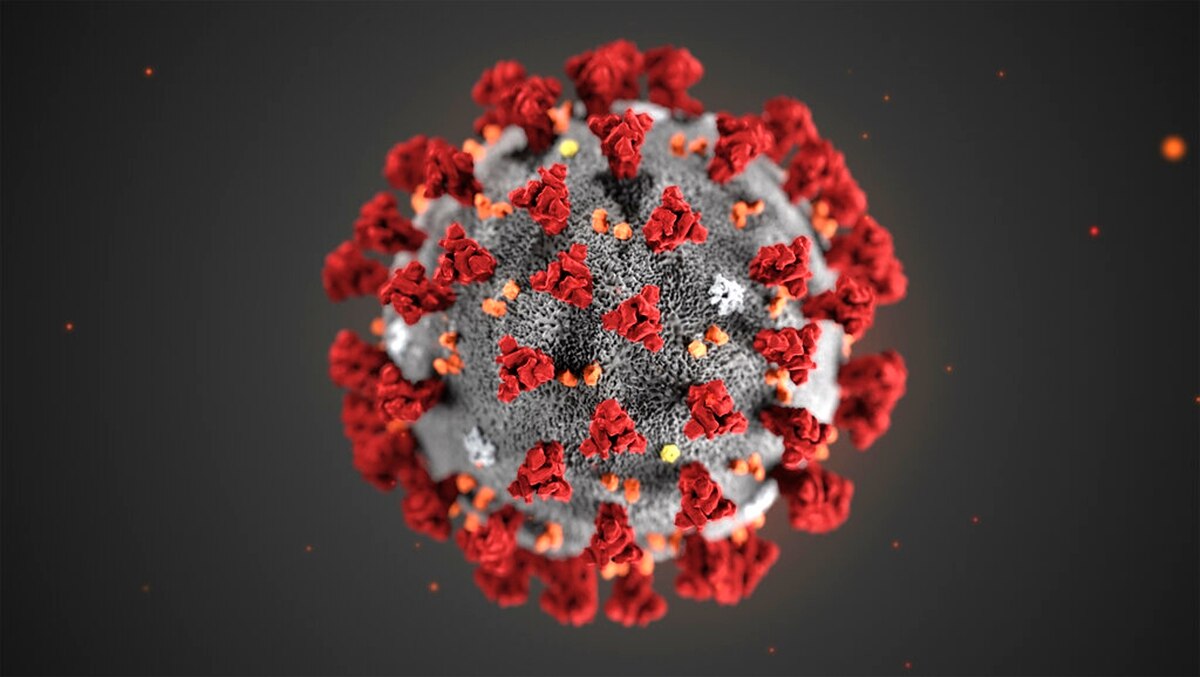
The delta variant of the SARS-CoV-2 virus remains predominant in Wisconsin, but the omicron variant, which has been identified in the last month, is now spreading rapidly. At least 19 cases of omicron have been detected in the state. The omicron variant is highly contagious, Timberlake said, and it is expected “to cause a rapid increase in disease activity in our state in the coming weeks, just as it has in other states and other countries.”
Hospitals ‘pushed to the breaking point’
The Wisconsin Hospital Association (WHA) reported Monday that 1,660 people were hospitalized for COVID-19, about a 20% increase since the beginning of the month.
One out of four hospitalized COVID-19 patients is in intensive care, according to the WHA. More than 95% of ICU beds are full, with COVID-19 accounting for about one-third of those patients.
The new state health advisory points to the onset of the omicron variant and reiterates what DHS has been urging for months, but with even greater emphasis: Getting vaccinated against COVID-19, and for people who have already received the full vaccine regimen, getting a booster shot; wearing masks at indoor gatherings “regardless of vaccination status”; and getting tested for COVID-19 if a person has symptoms of the illness or has been exposed to someone with the virus.
“What each of us chooses to do in the next few weeks really matters,” Timberlake said. “There is a serious risk that continued increased numbers of COVID-19 cases will overwhelm an already strained health care system.”
A senior Marshfield Clinic physician-executive, who also spoke at Monday’s briefing, described conditions that came close to sounding overwhelmed already.
“It is important that everyone understands that our health care organizations have been pushed to the breaking point,” said Dr. William Melms, the Marshfield Clinic Health System’s chief medical officer. “And it is quite possible that omicron will push us beyond the breaking point.”
Across the nine-hospital Marshfield system, the number of hospitalized COVID-19 patients has grown by 10% in the last week. There are now 125, according to a Marshfield Clinic spokesman.
In a recent four-week period at the Marshfield hospital, 35 patients died from COVID. “In fact, the only reason that our COVID numbers haven’t risen as fast as they could have is because of the deaths from COVID within our facilities, “ Melms said.
Throughout the Marshfield system, which spans the central and northwestern part of the state, the vast majority of hospitalized COVID-19 patients and more than 90% of those who died were not vaccinated, he said.
“One of the great tragedies of this pandemic is the number of nearly preventable deaths, nearly completely preventable deaths, that we have throughout our state,” Melms said. He urged vaccination and attention to masking and other measures to reduce the spread of the virus.
Turning away patients
Melms also rejected the claim that Assembly Speaker Robin Vos (R-Rochester) made in a newspaper report published last week, that vaccine requirements at hospitals, clinics and nursing homes were to blame for their staff shortages.
Marshfield has a vaccine mandate and more than 12,000 employees. “We lost less than 100 employees because of the vaccine mandate.” Melms said. At the same time, “thousands of our [vaccine-] hesitant employees did elect to get vaccinated — so it accomplished what it needed to do.”
At the same time, however, he said, health care providers are striving not to shut down screenings for cancer and routine care for chronic medical conditions, hoping to avoid the delays that many patients experienced early in the pandemic, when hospitals put off routine but necessary care.
While lack of space is part of the problem hospitals face, the primary difficulty is staffing. “We can always create more space,” Melms said. “But we cannot create the people to care for our patients.” Marshfield has juggled staff assignments internally to fill vacancies and added health care workers from staffing agencies.
To help fill health care worker vacancies, the state has expanded its contract with staffing agencies, with 415 contract nurses and other health care workers now working at hospitals and long-term care homes in Wisconsin, Timberlake said. The state also remains in talks with the Federal Emergency Management Agency (FEMA) to place additional health care workers.
The state’s four facilities for long-term mental health patients have also experienced chronic staffing shortages, and Wisconsin National Guard members are helping to fill vacancies there, she said.
While urging Wisconsinites to wear masks to avoid spreading the virus, Timberlake didn’t directly answer a reporter who asked whether the department would ask local health departments to institute stronger public health protections, such as mask mandates.
“I think the important message today is that wearing masks is very effective at preventing the spread of COVID-19,” Timberlake said. She noted Dane County’s ongoing mask mandate — the only one in the state currently — as well as some employers and other places that require or urge masking to prevent the spread of the virus.
“We all need to be really depending on one another to take those steps to stop the spread of this important and very challenging virus,” Timberlake said.
Mask order extended; court allows new challenge
Wisconsin’s last statewide health order, a mask mandate that was part of a health emergency declaration, was canceled by a state Supreme Court ruling early in 2021. Since then the strongest public health orders have been left to local governments, and currently Public Health Madison & Dane County (PHMDC) is the only local agency that has a mask order.
Coinciding with the order, the Wisconsin Supreme Court announced Monday it would take a case brought by the Wisconsin Institute for Law & Liberty (WILL), challenging the county health department’s authority to issue health orders. WILL’s lawsuit argues that the orders require the Dane County Board’s assent.
The state statute conferring duties on local health officers makes no mention of requiring any approval by county boards or other local legislative bodies.
The state Supreme Court granted WILL’s petition to bypass lower courts in a suit that the law firm filed in Dane County Circuit Court in January 2021. With Monday’s decision, the Supreme Court reversed an earlier decision, when the justices voted 4-3 in November 2020 to reject WILL’s first attempt to take the case straight to them.
The court’s action also departs from its 4-3 ruling in August that denied WILL’s attempt to bypass lower courts in a challenge specifically to the Dane County mask order.
WILL has played a role in several court cases that have blocked public health measures and hobbled local and state health authorities, including the ruling that ended Wisconsin’s statewide mask order.
Pressure builds on hospitals as COVID surges was originally published by the Wisconsin Examiner.
More about the Coronavirus Pandemic
- Governors Tony Evers, JB Pritzker, Tim Walz, and Gretchen Whitmer Issue a Joint Statement Concerning Reports that Donald Trump Gave Russian Dictator Putin American COVID-19 Supplies - Gov. Tony Evers - Oct 11th, 2024
- MHD Release: Milwaukee Health Department Launches COVID-19 Wastewater Testing Dashboard - City of Milwaukee Health Department - Jan 23rd, 2024
- Milwaukee County Announces New Policies Related to COVID-19 Pandemic - County Executive David Crowley - May 9th, 2023
- DHS Details End of Emergency COVID-19 Response - Wisconsin Department of Health Services - Apr 26th, 2023
- Milwaukee Health Department Announces Upcoming Changes to COVID-19 Services - City of Milwaukee Health Department - Mar 17th, 2023
- Fitzgerald Applauds Passage of COVID-19 Origin Act - U.S. Rep. Scott Fitzgerald - Mar 10th, 2023
- DHS Expands Free COVID-19 Testing Program - Wisconsin Department of Health Services - Feb 10th, 2023
- MKE County: COVID-19 Hospitalizations Rising - Graham Kilmer - Jan 16th, 2023
- Not Enough Getting Bivalent Booster Shots, State Health Officials Warn - Gaby Vinick - Dec 26th, 2022
- Nearly All Wisconsinites Age 6 Months and Older Now Eligible for Updated COVID-19 Vaccine - Wisconsin Department of Health Services - Dec 15th, 2022
Read more about Coronavirus Pandemic here