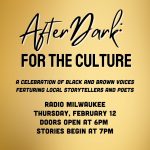
Anti-Fraud Law’s Repeal Hurts Taxpayers
State losing millions in federal settlements because Walker, GOP killed whistleblower law.

Gov. Scott Walker signs the 2015-17 Wisconsin state budget at Valveworks USA in Waukesha, Wis., on July 12, 2015. A provision in that document, approved by the Legislature with no debate, repealed the state False Claims Act. Because of that repeal, Wisconsin now collects millions of dollars less when companies are caught defrauding the state’s Medicaid program. Photo by Michael Sears/Milwaukee Journal Sentinel.
Wisconsin taxpayers have missed out on millions of dollars in settlements after state officials quietly eliminated one of the most effective tools for rooting out fraud in the $9 billion-a-year state Medicaid program, interviews and public records show.
It is a glaring exception to Republican Gov. Scott Walker’s crusade aimed at eliminating waste, fraud and abuse in state government.
That estimate was produced by the Wisconsin Center for Investigative Journalism using methodology endorsed by Taxpayers Against Fraud, a nonprofit organization that advocates for whistleblowers and government efforts to root out fraud. The state Department of Justice declined to estimate the loss.
Asked in an email why Walker repealed the law, spokesman Tom Evenson did not address the question but instead highlighted the governor’s efforts to root out fraud and waste in Medicaid and FoodShare, which he said have saved taxpayers an estimated $150 million. Evenson also did not respond to an offer to have the state estimate the losses from the repeal of the False Claims Act.
Said Evenson: “The bottom line is that Medicaid fraud continues to be investigated and detected.”
The law had awarded whistleblowers and their attorneys up to 30 percent of penalties when companies were caught defrauding the state’s Medicaid program. The national average in such cases is much less, however — about 16 percent.

Wisconsin is slated to receive $3.4 million as part of a nationwide settlement for allegedly underpaying rebates it owed to the Medicaid program with the makers of EpiPen, a drug used to counteract severe allergic reactions. A whistleblower organization calculates Wisconsin could have earned an additional $695,000 if lawmakers and Gov. Scott Walker had not repealed the state’s False Claims Act in 2015. Photo by Coburn Dukehart / Wisconsin Center for Investigative Journalism.
Business groups, which pushed Walker and the Legislature to repeal the law, derisively refer to such whistleblowers and their attorneys as “bounty hunters.”
In October, Republican Attorney General Brad Schimel announced that the state will receive $3.4 million of a nationwide settlement against the makers of EpiPen for allegedly underpaying rebates it owed to the Medicaid program, which is jointly funded by the state and federal governments.
“Mylan just discovered taking advantage of taxpayers comes at a high price,” Schimel said in a statement announcing the settlement involving EpiPen, which is used to counteract severe allergic reactions.
But the price Mylan will pay is tilted more toward reimbursing the federal government than giving money back to Wisconsin taxpayers, thanks to the repeal of the state False Claims Act in the 2015-17 state budget. That decision made Wisconsin ineligible for a larger share of the settlement, resulting in an estimated $695,430 less for the state in the EpiPen settlement, said Patrick Burns, associate director of Taxpayers Against Fraud.

Stephen Kohn, head of the Washington, D.C.-based National Whistleblower Center, says because of the repeal of the state’s False Claims Act, Wisconsin is one of the worst states for whistleblowing. Photo courtesy of Leslie Rose.
Said Burns: “It starts to look like real money.”
Stephen Kohn, executive director of the National Whistleblower Center, said Wisconsin is the only state to repeal its False Claims Act, a distinction he believes makes it one of the worst states in the country for whistleblowers.
Over the past 30 years, 88 percent of fraud cases brought on behalf of the U.S. Department of Health and Human Services, which runs Medicaid, were filed by whistleblowers, according to figures provided by the U.S. Department of Justice. Between 1987 and 2016, the government initiated 907 cases, while whistleblowers brought 6,683 cases.
Such whistleblower cases, known as qui tam cases, also brought in more money than those launched by the government. Whistleblower cases filed on behalf of HHS brought in $27.8 billion to the federal government, with $4.6 billion going to whistleblowers and their attorneys. Cases initiated by the government brought in $6.1 billion. The figures do not include billions of dollars returned to states, nor do they include criminal fines levied against the companies, according to Taxpayers Against Fraud.
Repeal stymies multi-million-dollar suit
Efforts by former Democratic Wisconsin Attorney General Peg Lautenschlager, to recoup millions of dollars for the state for other alleged prescription drug overbillings also have been thwarted — at least for now — by repeal of the act.
A Dane County Circuit Court judge ruled in May that Lautenschlager’s lawsuit against a group of pharmaceutical companies cannot proceed because it was filed after the Legislature repealed the state False Claims Act — although the alleged behavior occurred years earlier, from 2002 through 2011. Lautenschlager filed the case as a private citizen.

Former Wisconsin Attorney General Peg Lautenschlager has filed a whistleblower lawsuit against a handful of drug companies, alleging they overcharged the state’s Medicaid system between 2002 and 2011. The current attorney general, Brad Schimel, has declined to join the suit. Here, Lautenschlager receives a lifetime achievement award from the Democratic Party of Wisconsin on Oct. 10, in Madison, Wis. Photo by Brian Evans / Democratic Party of Wisconsin.
Lautenschlager has appealed that decision. The defendant drug companies — Actavis Mid Atlantic, Actavis Elizabeth, Par Pharmaceuticals, Teva Pharmaceuticals USA, Forest Laboratories and Forest Pharmaceuticals — argue Judge Juan Colas got it right; such whistleblower cases are now barred in Wisconsin.
If the state’s former top prosecutor is successful, the companies would be forced to repay state taxpayers, and — under the old False Claims Act — an as-yet undetermined percentage would go to Lautenschlager and her attorney, former Deputy Attorney General Dan Bach.
But the current attorney general, Schimel, has declined to participate in the litigation. That means Lautenschlager and Bach must bear the cost — and the risk — of pursuing the case.

Wisconsin Attorney General Brad Schimel has railed against companies that defraud the state. But he also has declined to intervene on behalf of a whistleblower case that could results in tens of millions of dollars from prescription drug companies for allegedly overcharging the state’s Medicaid program. Here he is seen at the State of the State address at the state Capitol in Madison, Wis., on Jan. 10. Photo by Coburn Dukehart / Wisconsin Center for Investigative Journalism.
“If we do not prevail on our appeal, the state will lose the opportunity to collect tens of millions of dollars,” Bach said. “The state settled all of the cases that were brought while Peg (Lautenschlager) was AG and collected a bundle.
“There is no good reason why the state would repeal a statute … that allows it to recover funds fraudulently obtained from the public,” he continued. “The repeal was done on one line in the middle of the massive budget bill. No debate, no explanation.”
Schimel spokesman Johnny Koremenos said the state had several reasons for declining to intervene, including that it “disagreed with the merits of the claim.”
“Even if the claims were meritorious and not stale and old, the state would still be entitled to at least 70 percent of the proceeds even after declining,” Koremenos wrote. “The state would have had little to gain from intervening in this lawsuit. Furthermore, there was no indication that defendants were amenable to settlement.
“We did not see that the resources needed to litigate these cases was worth the litigation risk.”

Former Wisconsin Deputy Attorney General Daniel Bach questions why the state repealed its False Claims Act and why it now declines to take up a case that could mean tens of millions of dollars in reimbursements to the state’s Medicaid program. Bach has brought a whistleblower lawsuit against a handful of pharmaceutical companies along with former Attorney General Peg Lautenschlager. Photo courtesy of Lawton and Cates.
Bach does not buy that argument. He noted that the state under Lautenschlager brought suit in 2004 against 36 pharmaceutical companies “based on similar facts and the same legal theory” as the current case. After years of litigation, the case against Pharmacia resulted in a judgment of roughly $30 million.
“All of the other defendants wound up settling with the state, resulting in the recovery of tens of millions of dollars from defendants who had defrauded the state Medicaid program,” said Bach, who was Lautenschlager’s second-in-command at the time the original suit was filed.
In one of those settlements — inked by Schimel just last year — the DOJ settled with a handful of drug companies for $60 million, $10 million of which went to Miner, Barnhill and Galland, the law firm that had initiated the suit. The alleged overcharging of Medicaid, including the BadgerCare and SeniorCare programs, stretched back to 1993, according to the settlement.
Said Bach: “There is no statute of limitations or ‘staleness’ issue. Whatever reasons DOJ may have had for declining the opportunity to intervene in the current case, the lack of merit of these claims cannot plausibly be among them.”
Anti-fraud law weakened — then killed
The death of the state False Claims Act came in stages beginning in 2011, the year Walker was elected.
That year, federal officials notified Wisconsin that it must update its False Claims Act to meet new requirements or forfeit the extra 10 percent share of recoveries to the Medicaid program that states with qualifying False Claims Acts receive. The state declined.

Gov. Scott Walker signed the 2015-17 budget that eliminated the state’s False Claims Act, which had provided incentives to whistleblowers and extra money for the state in cases of Medicaid fraud. Here he greets State Superintendent of Public Instruction Tony Evers prior to delivering his budget address at the State Capitol in Madison, Wis., Feb. 8. Photo by Coburn Dukehart / Wisconsin Center for Investigative Journalism.
Wisconsin was granted a two-year grace period to update the law but failed to do so, leading the state to become ineligible for the incentive payments beginning in 2013, the state Department of Justice confirmed.
Then in 2015, as part of the state’s two-year budget, the Legislature repealed the law, which had provided potentially millions of dollars in monetary incentives to both the state and whistleblowers who report Medicaid fraud.
The law — repealed with the encouragement of Wisconsin Manufacturers and Commerce, the state’s largest business lobby — had allowed individuals and their attorneys, called “relators,” to receive a portion of the penalty, depending on their contribution to uncovering the fraud.
Now that the state no longer has a False Claims Act, whistleblowers in Wisconsin have less incentive to come forward with fraud allegations — and the state is getting less money, according to attorneys who represent whistleblowers.
“Anyone who has weakened this law or repealed it is giving a green light to people to steal from the Wisconsin taxpayer,” said Kohn, whose National Whistleblower Center is a legal advocacy association for whistleblowers. “Now the most important tool for discouraging and preventing those rip-offs (at the state level) has been eliminated.”
False claims laws targeted
Wisconsin’s law was enacted in 2007 after passage of the 2005 federal Deficit Reduction Act, which gave states that enacted False Claims Acts higher recoupments in Medicaid fraud cases.
Thirty states have such laws; as of 2015, 13 states had laws that qualified them to receive additional payments when their Medicaid programs are defrauded, according a Seton Hall Law School study.

Rep. John Nygren, R-Marinette, as co-chairman of the Legislature’s Joint Finance Committee, helped to repeal the state’s False Claims Act as part of the 2015-17 state budget. He is seen here in the Assembly Chambers at the Capitol, in Madison, Wis., Sept. 24, 2015. Photo by Michelle Stocker / The Cap Times.
Nationally, there has been a coordinated effort by business groups — particularly those representing government contractors — to prevent states from adopting False Claims Acts. In West Virginia, lawmakers voted down a proposed law after the state’s Chamber of Commerce lobbied against it.
After Wisconsin’s Legislature killed the state False Claims Act, Burns wrote, “At a time when 25 percent of Wisconsin’s budget is being spent on Medicaid, winking at fraud in that system is the height of fiscal irresponsibility.”
Money recovered under the state’s False Claims Act is shared between the state and the federal government, which both fund Medicaid.
When Wisconsin’s law was still compliant, the whistleblower and his or her attorney would receive their shares, with the remainder split about 50-50 between the state and the feds. But after it refused to update the law, Wisconsin became eligible for just about 40 percent of the share of the recoveries.
To illustrate the financial impact, if the state were defrauded of $20 million, Wisconsin and the federal government could recover $60 million from the company or individual responsible since both the old state law and current federal law call for triple damages in such cases.
Under the old state law, Wisconsin and the federal government would have each received $24.9 million — with the remaining up to $10.2 million going to the whistleblower and the whistleblower’s attorney.
 Wisconsin Manufacturers and Commerce, the powerful business lobby, pushed Gov. Scott Walker and the Legislature to repeal the state False Claims Act, which allowed whistleblowers and their attorneys who identified fraud in the state’s Medicaid system to collect a portion of proceeds. Lawmakers repealed the law without debate in the 2015-17 budget, which Walker signed. Photo by Riley Vetterkind / Wisconsin Center for Investigative Journalism.[/caption]
Wisconsin Manufacturers and Commerce, the powerful business lobby, pushed Gov. Scott Walker and the Legislature to repeal the state False Claims Act, which allowed whistleblowers and their attorneys who identified fraud in the state’s Medicaid system to collect a portion of proceeds. Lawmakers repealed the law without debate in the 2015-17 budget, which Walker signed. Photo by Riley Vetterkind / Wisconsin Center for Investigative Journalism.[/caption]
During the 2015-16 legislative session, Wisconsin Manufacturers and Commerce went a step further, calling for repeal of the law. The group charged that the False Claims Act provided “an incentive for private attorneys to sue businesses for alleged fraud” and that the state should, “instead, maintain this authority with the experienced investigators within the state Department of Justice.”
WMC did not respond to requests for an interview.
“By awarding the person who brings a private cause of action a sizable portion of the proceeds, (the act) reduces the amounts recovered for the state’s Medical Assistance program,” the group’s president, Bill Smith, claimed in a 2015 letter to Walker.

Sen. Alberta Darling, R-River Hills, as co-chairwoman of the Legislature’s Joint Finance Committee, helped to repeal the state’s False Claims Act as part of the 2015-17 state budget. She is seen during Gov. Scott Walker’s budget address at the State Capitol in Madison, Feb. 8, 2017. Photo by Coburn Dukehart / Wisconsin Center for Investigative Journalism.
The governor did not propose repeal in his budget, but the Legislature did. Walker, who had the option of vetoing the repeal, left it intact.
No committee discussion or debate occurred over the 2015 repeal. The motion was introduced in the Legislature’s Joint Finance Committee by co-chairs Rep. John Nygren, R-Marinette, and Sen. Alberta Darling, R-River Hills. They did not respond to several requests for comment.
Lisa Rickard, president of the U.S. Chamber Institute for Legal Reform, applauded Walker for signing the repeal into law, saying it would stop incentivizing “private bounty hunter plaintiffs” and was more efficient since it left prosecuting such fraud solely in the hands of the state.
State loses out multiple ways
State officials declined several requests to calculate the amount of money Wisconsin may have lost since the law became non-compliant or to verify the Center’s calculations.
Lautenschlager said it is difficult to estimate the total loss, since the amount would depend on the size and number of cases brought each year. Another factor would be whether or not a whistleblower was involved and to what extent.

Attorney Nola Hitchcock Cross, who has represented whistleblowers, says repeal of the state False Claims Act was prompted by “corporate greed.” Wisconsin Manufacturers and Commerce had urged the state to do away with the law, which allowed whistleblowers and their attorneys who identified fraud to collect a portion of proceeds when companies were caught cheating the state’s Medicaid program. Photo courtesy of Nola Hitchcock Cross.
But she has no doubt the state is forfeiting a significant amount of money and that whistleblowers are less likely to initiate actions.
“Clearly, the numbers would be at least one-third less than under the old law,” Lautenschlager said, referring to the loss of the 10 percent incentive. In addition, “there is much less incentive to spend the money to bring a case if damages are reduced.”
She rejected the argument that Wisconsin’s law benefited only private plaintiffs.
Opponents said “all it was was a way for trial attorneys to get rich, even though a whole bunch of the money went to the government,” Lautenschlager said.
Nola Hitchcock Cross, a Milwaukee attorney who has won multimillion-dollar settlements involving Medicaid and Medicare fraud nationally, said there is less financial incentive now to report Medicaid fraud in Wisconsin than in some other states.
Asked why she believed Wisconsin repealed its False Claims Act, Cross responded: “Corporate greed.”
“There isn’t an interest in preserving taxpayer funds regarding Medicaid,” Cross said, adding that eliminating the law “shoots the taxpayer in the foot.”
Fraud tips continue to come in
But according to Assistant Attorney General Katie Wilson, the state’s Medicaid Fraud Control and Elder Abuse Unit still receives referrals from many sources, including a hotline set up for tipsters. After dipping for a few years, settlements were up in fiscal year 2016 — although, the Center found, not as much as they could be if the state had a False Claims Act.
Of the $81 million recovered by the Medicaid fraud unit in 2016, Wisconsin recovered $20.9 million under False Claims Act theories. According to a calculation endorsed by Taxpayers Against Fraud, that amount could have been $26.2 million if Wisconsin had its own False Claims Act in compliance with the federal law. Officials at the Medicaid fraud unit would not confirm these numbers.
Wilson declined to provide an opinion as to whether the state is recovering less because of the law’s repeal. Morgan, of the Legislative Fiscal Bureau, said it is unknown what the impact of the law’s repeal has been.
Tim Samuelson, then-director of the Medicaid fraud unit, said there has not been enough time without the law to determine if it is affecting people’s willingness to expose Medicaid fraud. Samuelson has since been appointed by Walker to a vacancy on the Dane County Circuit Court.
“What I see is that we still get citizen complaints; we still get complaints from former employees of facilities,” Samuelson said. “I know that many of these cases are still being filed under the repealed act based on facts that arose prior to repeal, so we’re still getting those types of cases, and I don’t know that there’s been enough time for us to have an opinion as to any causes or results from repeal.”
Reporter Cara Lombardo contributed to this story, which was produced as part of an investigative reporting class in the University of Wisconsin-Madison School of Journalism and Mass Communication under the direction of Dee J. Hall, the Wisconsin Center for Investigative Journalism’s managing editor. The nonprofit Center (www.WisconsinWatch.org) collaborates with Wisconsin Public Radio, Wisconsin Public Television, other news media and the UW-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by the Center do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.
Broken Whistle
-
Doctors Side Against Injured Public Workers?
 Jan 21st, 2018 by Alexandra Hall and Dee J. Hall
Jan 21st, 2018 by Alexandra Hall and Dee J. Hall
-
Did State Retaliate Against Whistleblowers?
 Dec 5th, 2017 by Leo Vartorella
Dec 5th, 2017 by Leo Vartorella
-
Court Ruling Weakens Whistleblower Law
 Dec 4th, 2017 by Bobby Ehrlich
Dec 4th, 2017 by Bobby Ehrlich




















There is almost certainly some complexity here, and, therefore, the long article. But the basic issue is pretty straightforward. In a corporate controlled plutocracy, like the State of Wisconsin, there are only two values that count. These are shareholder/owner value and executive compensation. To sustain these values, sometimes it is necessary to either skirt the law or commit fraud or some other crime, such as unleashing the opioid epidemic, destroying the environment or producing a global financial collapse.
Consequently, there is a need to take steps to avoid being held accountable. Worst case scenario: fraud and criminality, regardless of how many people are harmed, must be “punished” by a “negotiated settlement,” with “no acknowledgment of guilt,” and certainly no criminal accountability for executives or boards.
But why even have the minimal threat posed by whistle blower laws around to make people slightly nervous? Better to just get rid of the law, as quietly as possible.
Here is an exercise. Watch any commercial television network for one hour. Do not watch the programs, only the commercials for pharmaceuticals, banks, ambulance chasers, cars, telecommunications companies, insurance and the “But Wait!” junk peddlers. Afterward, name one industry or company in that hour that you trust. Then, put on Fox News and it gets even better because you can learn how to buy gold/silver before the inevitable hyperinflation and protect yourself from the equally inevitable home invasion.
Since television and social media haven’t yet totally lobotomized us, there is a need to protect corporations and their wealthy shareholders from the threat of punishment for the various corporate frauds, scams and crimes. The best way is to make sure that they are never revealed. Wisconsin’s government is, as always, happy to oblige, and the State is again leading the way into the plutocratic wilderness by getting rid of this potentially onerous provision.
Oh what a tangled and crooked web Walker weaves…