State’s ACA Insurance Exchange Enrollment Up This Year
Nationally new record set, with 12% increase, up to 16.3 million people enrolled.
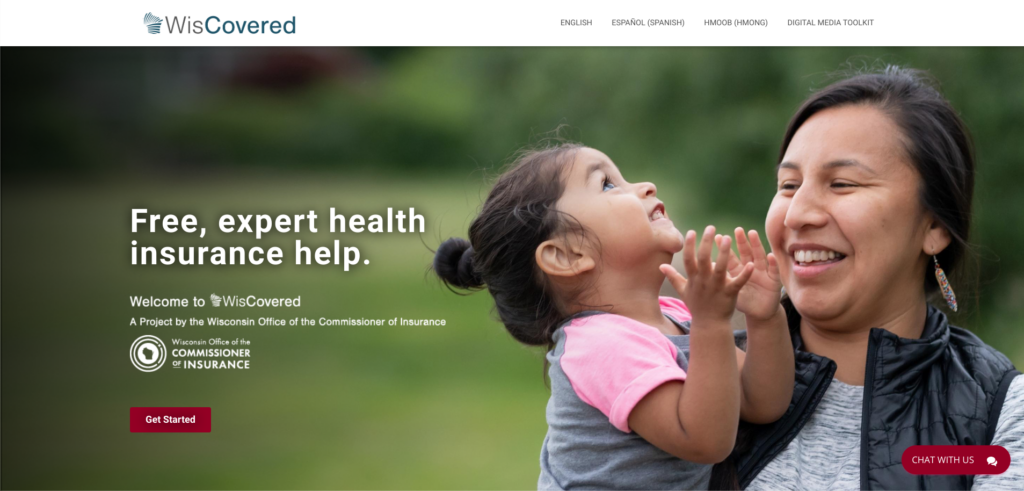
The Office of the Commissioner of Insurance (OCI) maintains the website WisCovered.com to help people seeking health coverage. (Screenshot)
For all of her adult life, the federal Affordable Care Act has made a big difference for Kat Klawes.
“I have never had a traditional job that has offered health care benefits,” says Klawes, who lives in Milwaukee. She’s mostly been self-employed as an independent contractor for small nonprofit and education organizations.
Thanks to the ACA, she was covered by her parents’ health insurance until she turned 26 five years ago. Since then, she’s been able to buy health insurance on Healthcare.gov, the federal health insurance exchange that the ACA created.
“The health care exchange allows me the freedom to be self-employed,” says Klawes. “I am more easily able to find a health care plan that meets my unique needs.”
Klawes got more company when she renewed her health insurance plan in the most recent Healthcare.gov open enrollment period that concluded in January.
According to federal and state officials, this year 221,128 Wisconsin residents signed up for health coverage through the federal health insurance exchange, Healthcare.gov — almost 9,000 more than the open enrollment period at this time in 2022. Nationwide, a record 16.3 million people signed up this year, a 12% increase from a year ago, according to Protect Our Care, an Affordable Care Act advocacy organization.
Setting standards, making insurance affordable
The ACA created the exchange to make it easier for individuals and small businesses to buy their own health insurance plan from a list of qualifying private insurers. The marketplace was one of several interconnected elements to the act, which set minimum standards for health insurance plans nationally and also outlawed the practice of denying coverage or charging higher premiums for people with a pre-existing health condition.
The ACA standards cover health insurance offered as an employee benefit as well as plans sold on the marketplace, which was established primarily for people for whom employment-based health coverage isn’t available.
The Biden administration also ended the so-called family glitch that made it harder for some families to qualify for premium subsidies. All of those initiatives “made health care through the ACA marketplaces more affordable than ever before,” says Protect Our Care’s Joe Zepecki.
In addition, the Biden administration boosted funding for the ACA Navigator program, which provides guidance to consumers using Healthcare.gov. According to Protect Our Care, the added resources have made it possible to reach out to underserved communities including racial and ethnic minorities, rural residents and the LGBTQ community.
Wisconsin Insurance Commissioner Nathan Houdek also credits a website, WisCovered.com, that the Office of the Commissioner of Insurance (OCI) and the Department of Health Services (DHS) established in 2020 as another entry point for consumers to seek coverage. According to OCI, more than 43,000 Wisconsin residents visited WisCovered.com in the latest open enrollment period.
“We are proud of our competitive and reliable health insurance market in Wisconsin and glad to be able to provide a resource like WisCovered.com to share information about that marketplace and connect consumers with enrollment assistance,” Houdek said in an OCI statement Jan. 26.
Tax credits boost enrollment
The extended tax credits helped spark stronger interest in buying a health plan through Healthcare.gov, says Adam VanSpankeren, who manages the Navigator program for the nonprofit Covering Wisconsin.
VanSpankeren says it was an important priority at Covering Wisconsin to get the message out that “the [Healthcare.gov] marketplace is more affordable than ever, especially in areas with more than one plan” to choose from. The Navigator program has been sharpening its marketing messages in the last few years so that it can reach more people who need health insurance, he says.
Klawes saw the impact of the higher subsidies firsthand.
Before they were enacted, “I was paying around $250 a month” for her health insurance premium, she says.
In 2022, the subsidy pulled her premium cost down to less than a dollar a month. Her current premium is about $50 a month after the subsidy.
That’s also made it possible for her to afford a plan with a lower deductible and lower annual out-of-pocket maximum, which now will top out at $1,050 a year if she goes to a provider in her insurer’s network, and $1,900 a year if she goes to out-of-network providers.
The program isn’t perfect, she acknowledges. The hearing aids she requires aren’t covered, for example. “My hope is for the ACA plans and the ACA is for some of it to be expanded” in what it covers, she says.
Nevertheless, “If I was not able to use an ACA plan it would significantly limit my job opportunities,” Klawes says. “I would be forced to work for corporations or large organizations who had more robust health care plans.” In a world without the ACA’s protections, a small employer might face losing its insurance coverage because of her more costly health care requirements.
New demand around the corner
While the general open enrollment period has now ended, people who need health insurance after a change in circumstances — such as losing a job with health coverage or a change in family status — can enroll on Healthcare.gov at other times during the year.
VanSpankeren says Covering Wisconsin is gearing up for a potential new rush in the coming months.
In March, the federal government will resume requiring Medicaid recipients to renew their eligibility for the health insurance program for the first time in three years. The renewal requirement was suspended in March 2020 as part of the federal health emergency to ensure that people had health care coverage in the COVID-19 pandemic.
During that period, Wisconsin’s Medicaid rolls have grown from less than 1.2 million people to more than 1.6 million as of December, according to DHS data. That includes people who are covered by BadgerCare, the health insurance plan for families and single adults with incomes at or below the federal poverty guidelines.
In passing the year-end federal spending bill in December 2022, Congress ended the renewal waiver effective in March. That will trigger a Medicaid enrollment “unwinding” starting in May, with tens of thousands of recipients every month having to prove they are still eligible and renew — or else be taken off the program and find new health coverage.
It’s not clear yet how many people will lose coverage. For those who do, the federal government has already announced an extended enrollment period on Healthcare.gov for people who have to leave Medicaid.
“We are preparing — more so than we would for an open enrollment period,” VanSpankeren says. “We’re expecting to be very busy during that time.”
Healthcare.gov enrollment breaks record in U.S., increases in Wisconsin was originally published by Wisconsin Examiner