Inside BRAVE, Milwaukee’s Expanding Clinic for Invisible Wounds
Veterans and first responders with PTSD and brain injuries find team-based, low-cost care at a new, larger location.
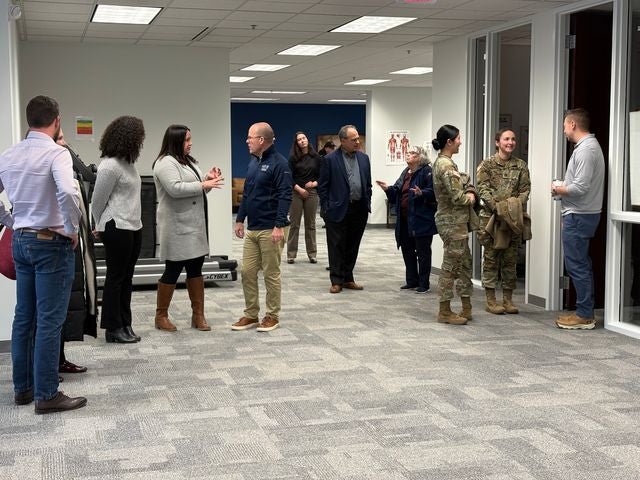
People gather during an open house at the new site of the Building Resilience through Action in Veterans and First Responders program in Wisconsin. Photo courtesy of the Medical College of Wisconsin
Johnathan Rose served in the United States Marine Corps for over 20 years.
In 2010, he was wounded from an IED blast during his deployment to Afghanistan. The explosion scarred parts of his body and left him blind in one eye.
The Virginia resident said he suffers from post-traumatic stress disorder. For the past few weeks, he’s been receiving treatment through a new Wisconsin program aimed at treating traumatic brain injuries and PTSD in veterans and first responders.
The three-week outpatient program, which is the first of its kind in the Midwest, is tailored to the needs of each patient.
“So it’s kind of not just learning, ‘oh, let’s deal with trauma, let’s do this’ — it’s putting all those pieces to the puzzle all together,” Rose said.
The program is called Building Resilience through Action in Veterans and First Responders and shortened to BRAVE. It was created in 2023 through a $12.5 million donation from the national nonprofit Avalon Action Alliance.
In Wisconsin, it is an initiative of the Wisconsin Institute of NeuroScience, which is a partnership of Children’s Wisconsin, the Froedtert & the Medical College of Wisconsin health network, the Medical College of Wisconsin and the Clement J. Zablocki VA Medical Center.
But the program recently moved to a new location at the Milwaukee County Research Park, which is more than triple the size of its former facility in Greenfield. The move will allow more patients to be treated.
“So we’re trying to grow to keep up with all the demand,” said Dr. Gregory Burek, the medical director of the BRAVE program. “And that’s been one vet (veteran) to another, getting the word out that it’s okay to get treatment, this is a real thing, and this is the place to do it.”
Sixty-one people have completed the program since February of 2024, while nearly 160 people have finished the three-day evaluation to be admitted. Burek said two teams are already working at the new space, and they’re working on adding a third team now.
Burek, a veteran himself, said there is often a stigma from veterans and first responders against getting mental health treatment or treatment for what he called the “invisible wounds,” or traumatic brain injuries and PTSD.
The Mayo Clinic found that symptoms of PTSD can include “flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the (traumatic) event.” Symptoms of traumatic brain injuries can include anxiety, depression, difficulty sleeping, dizziness, mood swings and headaches, among other symptoms, according to a statement from the Medical College of Wisconsin.
During the evaluation, the patient meets with physical therapists, speech therapists and psychologists, “to really get a full picture of the vet, the symptoms they have and the things that they’ve been dealing with,” Burek said.
“This is unlike anything that I’ve seen in medicine in the past,” Burek said. “This is all the docs talking to each other. This is really like whole health care, looking at what the vet is going through, from all of these different angles.”
Rose said he’s enjoyed meeting individually with counselors as part of the program.
“(It’s) bringing up a lot of stuff that I’ve never thought about, like stuff from childhood, stuff from deployment,” Rose said. “I’d rather get it out here than around my wife, my 5-year-old, because all you keep doing is pushing that down — eventually it’s going to come out somewhere.”
Burek said about half of the people they have evaluated and treated so far are Wisconsin residents. He also said around half of the staff on the teams are veterans themselves, which Rose said was important for him during his evaluation.
“So I got here and people were like, ‘we get what you’re saying, we understand what you’re saying, that is not wrong to feel,’” Rose said.
In an email, Medical College of Wisconsin spokesperson Colleen McDonald wrote that the program is offered at “little to no cost” for participants.
“The donation from Avalon Action Alliance helped us establish and buildout the BRAVE program in Milwaukee,” McDonald wrote. “It also helps reduce barriers to care for program participants, including financial barriers that might exist for participants who are traveling far from home to join the program.”
Wisconsin program treating brain injuries, PTSD for veterans and first responders is expanding was originally published by Wisconsin Public Radio.
If you think stories like this are important, become a member of Urban Milwaukee and help support real, independent journalism. Plus you get some cool added benefits.