Finally, Mental Health Care System Improving
Decades overdue, system is moving toward more community care and less overload at county mental health care complex.

Dan Baker, program director at the Crisis Resource Center, helps patients avoid visits to the county’s Mental Health Complex or other hospitals. (Photo by Matthew Wisla)
An average day for Sarah would be most people’s worst nightmare.
Haunted by schizophrenia her whole life, she was often confused, homeless, hungry and desperately alone. When her disorder pushed her into crisis the police or an emergency room doctor would refer Sarah (not her real name) to the Milwaukee County Mental Health Complex, 9201 W. Watertown Plank Road.
In her early 40s, she had been admitted into county care more than 40 times.
For Sarah, the cycle of crisis-treatment-release-crisis was only broken this summer after she began receiving treatment in the North Side community where she has been living. Because she always arrived at the county hospital in a state of crisis and was released with a new prescription as soon as it subsided, the county staff had almost never seen Sarah when she was not in crisis.
Doctors say the change transformed Sarah’s life. Regular visits with her doctors and a case coordinator have helped manage her schizophrenia, and Sarah gets the medical attention and other resources she needs to live a more ordered, balanced life.
Sarah’s case may represent a new normal for mental healthcare in Milwaukee if the county can deliver on its current plan. Following years of stagnation, mental healthcare delivery is transitioning from a long-standing reliance on centralized, county services to a new county-led but community-driven approach.
Sarah’s care is being coordinated through a new Crisis Resource Center in the Hampton Heights neighborhood at 5409 W. Villard Ave., which is under contract with the county. The 12-bed facility opened in August, has a staff of 24 mental healthcare professionals and is operated by the Milwaukee Center for Independence, a non-profit focused on assisting people with special needs. It represents the dramatic shift in mental healthcare taking place in Milwaukee County.
“We are moving towards the new model and working on being more person centered and improving patient satisfaction. But a lot more work still has to be done,” said Héctor Colón, Milwaukee County director of health and human services.
New model for care
Establishing resources in communities has been shown to increase efficiency, as well as quality of care and quality of life for patients, a rare win-win-win in the mental healthcare field, according to experts. The approach has proven itself across the country in cities such as Pittsburgh, New York and Houston.
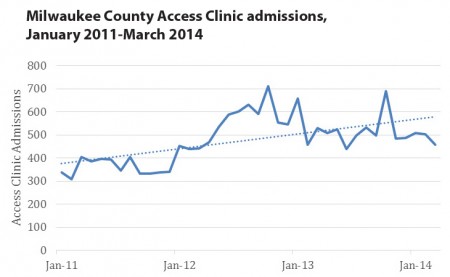
Milwaukee County is currently reducing the number of hospital beds and services it manages for mental healthcare patients while bed counts and service capacity increase in private hospitals and community clinics. At the same time, use of community-based resources, including admissions to Milwaukee County’s Access Clinic, are on the rise.
As services in the community ramp up, people such as Sarah receive targeted, ongoing care along with access to additional support. “As we expand community services like the Crisis Resource Centers, it helps stabilize patients, connect them back to the community and get them home or into more stable environments faster,” said Colón. “Instituting these changes and making them permanent is our current priority.”
Last month, a new white paper released by the Public Policy Forum confirmed progress in mental healthcare. Both the report and Colón point to a 30 percent reduction in acute inpatient admissions at the county facility and a 14 percent reduction in emergency room visits for mental health-related issues between 2011 and 2013.
According to Colón, projections through 2015 show a 46 percent reduction in admissions and 25 percent fewer emergency room visits. Those results mimic national trends, as the number of patients in crisis and emergency room visits are declining thanks to new treatments and expanded community-based programming.
Milwaukee County has invested about $8 million in new or enhanced community services since 2011 and the current budget proposal for 2015 includes another $4.9 million. The community-based investments have been used primarily to help fund crisis resource centers, local access clinics and safe, supportive housing.
The Milwaukee County Behavioral Health Division is undertaking these changes following years of criticism for out-of-control costs and adherence to a behind-the-times mindset fixated on maintaining central control of the mental healthcare system.
Advances in care
Decentralizing mental healthcare delivery is possible today because patients can receive treatment and get better while living outside hospitals or institutions. “As treatments have advanced, people with mental illness now can live in communities,” said David Hughes, vice president of the Human Services Research Institute, which co-wrote the recent white paper report with the Public Policy Forum and the Technical Assistance Collaborative. “They can go to school or work, and they can live next door to you and I.”
Until the science and technology of treating mental illness advances further, the report says, some patients will require acute care in private hospitals or from the county. “However, a strong, accessible community-based system can reduce the frequency and duration of inpatient stays.”
A disorder such as Sarah’s is only one possible trigger that can set off a crisis and land someone in an emergency room. At the Crisis Resource Center on Villard a majority of patients are homeless and many have a history of substance abuse. These individuals are always at risk, where one misstep — perhaps a relapse into substance abuse — or a setback such as losing or forgetting their medicine or having it stolen on the street, can cause a mental health crisis and admission to a hospital.
A network of services
Crucial to the potential success of Milwaukee’s new mental healthcare system will be linkages among organizations in the community. “Instead of silos, we work off a ‘Never a Wrong Door’ approach,” said Dan Baker, program director at the Crisis Resource Center. “It’s a huge opportunity for us to be able to connect someone who comes to our door with another provider that has what they need. So people can navigate the system easily without being diverted or hitting a dead end.”
When making referrals, Crisis Resource Center staff members reach out to other organizations on behalf of patients to make connections. According to Baker, they never simply hand a patient a piece of paper with a list of phone numbers.
Since “no wrong door” is a new concept for some, Baker frequently meets with other organizations to coordinate efforts.
During the past 13 months Milwaukee’s two Crisis Resource Centers have helped connect patients to other organizations in the community more than 1,300 times. Safe, affordable housing is a frequent need, along with clinics for physical and mental health needs, substance abuse centers and support groups.
As Milwaukee County transitions to a new community resource-based system, Colón says success is being measured by tracking crisis incidents and inpatient stays, as well as sobriety and substance abuse rates and whether patients are getting the results they want.
But change is never easy. Milwaukee’s new community-based approach to mental healthcare is likely to fail if rebalancing is not accompanied by a new culture, according to mental health experts.
“Culture change has been really tough in many places around the country,” said Hughes. “Lots of staff training and education needs to be done to make it work.”
For the county, which has firmly controlled mental healthcare in Milwaukee for decades, decentralizing represents a broad culture shift for employees. “This is a huge change for us. Admittedly, it’s very hard,” Colón said. “Our staff has to move on to new ways of doing things.”
Colón said he is driving change through new training programs and by carefully screening new hires.
In the meantime, the changeover to a system with far fewer county resources continues. Last year the county announced plans to close its Hilltop Complex for patients with developmental disabilities by the end of this year, and a nursing home facility by the end of next year. Colón said both closures are on track.
This story was originally published by Milwaukee Neighborhood News Service, where you can find other stories reporting on fifteen city neighborhoods in Milwaukee.